Page 8 - WJOLS
P. 8
Sherif Z Kotb et al
Statistical Methods vatively. Liver abscess reported in four cases (2 with LURFA
and 2 with PRFA). Early hospital mortality (n = 4) reported
Data was analyzed using SPSS (Statistical Package for Social only with PRFA.
Sciences) version 10. Qualitative data was presented as number The late outcomes of this series are reported in Tables 6 to
and percent. Comparison between groups was done by Chi- 10. There was insignificant decrease in tumour volume in all
square test or Fisher’s exact test (FET). Kolmogrov – Smirnov patients (Figs 11 to 13). While significant decrease in level of
test, tested quantitative data for normality. Normally distributed tumour marker alpha-fetoprotein was reported more with
data was presented as mean + SD. Student t- test was used to LUSRFA (80% vie 53.3% with PRFA group), p- value was
compare between two groups. Non-parametric data was highly significant 0.033. There were 28 deaths (16 with PRFA
presented as min – max and median. Mann-Whitney test was and 12 with LUSRFA). Less local recurrence, and distant
used for comparison between groups. P < 0.05 was considered metastases were reported with LUSRFA (13.33% and 6.67%
to be significant.
vie 26.67% and 13.33% with PRFA). The overall survival was
RESULTS more with LUSRFA (60% vie 46.67%); also 2 years disease-
free survival was more with LUSRFA (53.33% vie 40% with
This series involved 63 patients from ages 32 to 64 years, all of PRFA group) (Table 10).
whom presented to OCMU for RFA. 46 males and 14 females Our study found that 75% of patients with Child-Pugh
(Table 1). Thirty patients were managed with percutaneous RFA stage – A , and 83.33% of patients with tumour size less than 3
(PRFA group), and 33 patients were planned to manage with cm, survived for 2 years, from them 29/32 (90.63%) has single
laparoscopic ultrasound guided RFA (on clinical, laboratory lesion (Table 11).
and radiological bases), but IOUS reveal that the tumour in
three patients were not candidate for RFA as it invade important DISCUSSION
pedicle and thus excluded from the study. Thus, each group
was of 30 patients. The outcomes of this series of LUSRFA and PRFA performed
11-17
The preoperative clinical, laboratory and radiological by OCMU were equivalent to those in the surgical literature.
findings in the studied groups were summarized in Tables 2 and The high rate of morbidity and mortality may be due to bad
3: The most common site was the right lobe (n = 44); both lobes liver conditions and early learning course.
were affected in two patients (3.33%). Tumours affect one Procedure related complications represent 10% (6.67% with
segment (n = 48), or two segments (n = 12). Tumours sizes were PRFA and 3.33% with LRFA), these included skin burn (n = 4),
less than 3 cm (n = 12) or 3 – 5 cm (n = 48). Child’s – A one patient developed a third-degreeskin burn during the tract-
(n = 16) or B (n = 44). ablation portion of a percutaneous procedure (this required
Intraoperative US do not change the operative plan except debridement and wound care), and port site hernia (n = 2). De
11
in three patients that were excluded from the study (Table 4). Baere, et al. reported a total of 25 adverse events with radio-
Intraoperative US do not change the operative plan except frequency ablations that performed percutaneously on 312
12
in three patients that were excluded from the study (Table 4). patients. Wood et al. reported skin burn in (8%) of patients
Hospitalization period, procedure related and early after RFA.
postoperative complications reported in the first month were Early major complications occurred within 30 days of the
significantly less in LUSRFA group, (Table 5). The average RF ablation represent 20% (all with PRFA), these included
hospital stay was 1.2 days (vie 3 days with PRFA), skin burn internal haemorrhage (n = 4), acute liver failure (n = 4) and liver
(n = 4), internal haemorrhage (n = 4) and Acute liver failure abscess (n = 4), that was successfullytreated with percutaneous
(n = 4) were reported only with PRFA, all were treated conser- drainage ± endoscopicallyplaced internal biliary stent. Livraghi
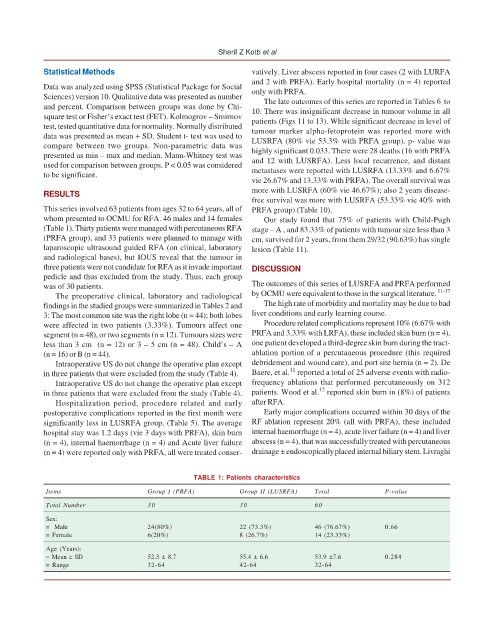
TABLE 1: Patients characteristics
Items Group I (PRFA) Group II (LUSRFA) Total P-value
Total Number 30 30 60
Sex:
= Male 24(80%) 22 (73.3%) 46 (76.67%) 0.66
= Female 6(20%) 8 (26.7%) 14 (23.33%)
Age (Years):
= Mean ± SD 52.3 ± 8.7 55.4 ± 6.6 53.9 ±7.6 0.284
= Range 32-64 42-64 32-64
6