Page 21 - WJOLS
P. 21
WJOLS
Pain and Cosmesis following Four-Port Laparoscopic Cholecystectomy: The Patient View
Statistical Method
Descriptive statistical analysis was undertaken on the data
obtained using Microsoft Excel 2007 (Microsoft Corpo-
ration, USA).
ReSuLTS
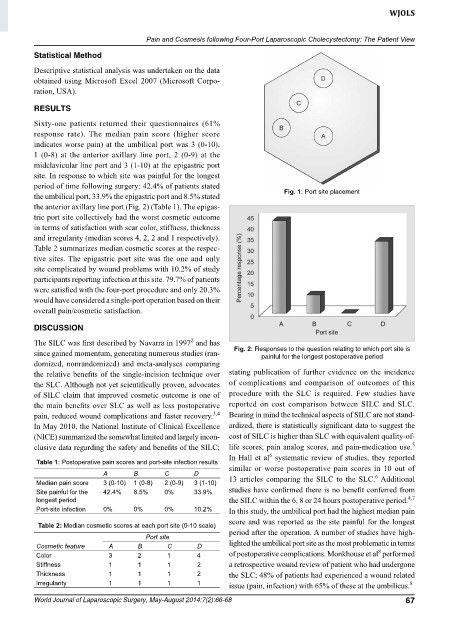
Sixty-one patients returned their questionnaires (61%
res ponse rate). The median pain score (higher score
indi cates worse pain) at the umbilical port was 3 (0-10),
1 (0-8) at the anterior axillary line port, 2 (0-9) at the
midclavicular line port and 3 (1-10) at the epigastric port
site. In response to which site was painful for the longest
period of time following surgery: 42.4% of patients stated
the umbilical port, 33.9% the epigastric port and 8.5% stated Fig. 1: port site placement
the anterior axillary line port (Fig. 2) (Table 1). The epigas-
tric port site collectively had the worst cosmetic outcome
in terms of satisfaction with scar color, stiffness, thickness
and irregularity (median scores 4, 2, 2 and 1 respectively).
Table 2 summarizes median cosmetic scores at the respec-
tive sites. The epigastric port site was the one and only
site complicated by wound problems with 10.2% of study
participants reporting infection at this site. 79.7% of patients
were satisfied with the four-port procedure and only 20.3%
would have considered a single-port operation based on their
overall pain/cosmetic satisfaction.
DISCuSSIoN
2
The SILC was first described by Navarra in 1997 and has
since gained momentum, generating numerous studies (ran- Fig. 2: Responses to the question relating to which port site is
painful for the longest postoperative period
domized, nonrandomized) and meta-analyses comparing
the relative benefits of the single-incision technique over stating publication of further evidence on the incidence
the SLC. Although not yet scientifically proven, advocates of complications and comparison of outcomes of this
of SILC claim that improved cosmetic outcome is one of pro cedure with the SLC is required. Few studies have
the main benefits over SLC as well as less postoperative reported on cost comparison between SILC and SLC.
pain, reduced wound complications and faster recovery. Bearing in mind the technical aspects of SILC are not stand-
3,4
In May 2010, the National Institute of Clinical Excellence ardized, there is statistically significant data to suggest the
(NICE) summarized the somewhat limited and largely incon- cost of SILC is higher than SLC with equivalent quality-of-
5
clusive data regarding the safety and benefits of the SILC; life scores, pain analog scores, and pain-medication use.
6
In Hall et al systematic review of studies, they reported
Table 1: Postoperative pain scores and port-site infection results
A B C D similar or worse postoperative pain scores in 10 out of
6
Median pain score 3 (0-10) 1 (0-8) 2 (0-9) 3 (1-10) 13 articles comparing the SILC to the SLC. Additional
Site painful for the 42.4% 8.5% 0% 33.9% studies have confirmed there is no benefit conferred from
4,7
longest period the SILC within the 6, 8 or 24 hours postoperative period.
Port-site infection 0% 0% 0% 10.2% In this study, the umbilical port had the highest median pain
score and was reported as the site painful for the longest
Table 2: Median cosmetic scores at each port site (0-10 scale)
Port site period after the operation. A number of studies have high-
Cosmetic feature A B C D lighted the umbilical port site as the most problematic in terms
8
Color 3 2 1 4 of postoperative complications. Monkhouse et al performed
Stiffness 1 1 1 2 a retrospective wound review of patient who had undergone
Thickness 1 1 1 2 the SLC; 48% of patients had experienced a wound related
Irregularity 1 1 1 1 issue (pain, infection) with 65% of these at the umbilicus.
8
World Journal of Laparoscopic Surgery, May-August 2014;7(2):66-68 67