Page 30 - World Journal of Laparoscopic Surgery
P. 30
Prachi Arora et al
Preparation In group II (Infertility) 12 (80%) out of 15 had shown
abnormal hysteroscopic finding as shown in Table 3. The
All patients were admitted in the hospital prior to the
procedure. Patients were kept nil orally since morning commonest finding observed on hysteroscopy was blocked
on the day of hysteroscopy. The patients were divided tubal ostia in 10 (66.6%) patients. In these cases, distending
into 2 groups: media was not seen passing through the ostia. In 9 out of
these 10 patients diagnostic laparoscopy was carried out,
Group a: Patients were given injection pethidine the tubes were confirmed to be blocked in 7 (77.7%).
50 mg IV and injection phenargan 25 mg IM.
In group III (Postmenopausal bleeding) 4 patients
Group b: general anesthesia—This group included (80%) out of 5 showed abnormal hysteroscopic findings.
patients who were very uncooperative or those who Atrophic endometrium was seen in 3 (37.5%) patients
needed concomitant surgery. and endometrial polyp was seen in 1 (12.5%) patients. In
All hysteroscopy examinations were carried out in
operation theater with 4 mm olympus telescope with Table 1: Indications for hysteroscopy and abnormal findings in
full aseptic precautions Saline was used as distending different groups
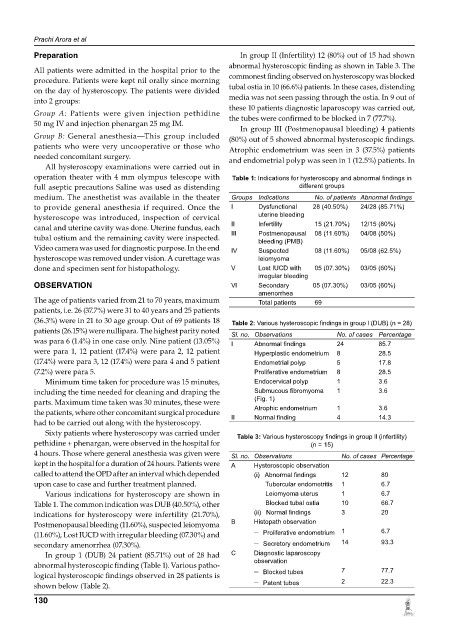
medium. The anesthetist was available in the theater Groups Indications No. of patients Abnormal findings
to provide general anesthesia if required. once the I Dysfunctional 28 (40.50%) 24/28 (85.71%)
hysteroscope was introduced, inspection of cervical uterine bleeding
canal and uterine cavity was done. Uterine fundus, each II Infertility 15 (21.70%) 12/15 (80%)
tubal ostium and the remaining cavity were inspected. III Postmenopausal 08 (11.60%) 04/08 (50%)
bleeding (PMB)
Video camera was used for diagnostic purpose. In the end IV Suspected 08 (11.60%) 05/08 (62.5%)
hysteroscope was removed under vision. A curettage was leiomyoma
done and specimen sent for histopathology. V Lost IUCD with 05 (07.30%) 03/05 (60%)
irregular bleeding
oBSERVATion Vl Secondary 05 (07.30%) 03/05 (60%)
amenorrhea
The age of patients varied from 21 to 70 years, maximum Total patients 69
patients, i.e. 26 (37.7%) were 31 to 40 years and 25 patients
(36.3%) were in 21 to 30 age group. Out of 69 patients 18 Table 2: Various hysteroscopic findings in group l (DUB) (n = 28)
patients (26.15%) were nullipara. The highest parity noted Sl. no. observations No. of cases Percentage
was para 6 (1.4%) in one case only. Nine patient (13.05%) I Abnormal findings 24 85.7
were para 1, 12 patient (17.4%) were para 2, 12 patient Hyperplastic endometrium 8 28.5
(17.4%) were para 3, 12 (17.4%) were para 4 and 5 patient Endometrial polyp 5 17.8
(7.2%) were para 5. Proliferative endometrium 8 28.5
Minimum time taken for procedure was 15 minutes, Endocervical polyp 1 3.6
including the time needed for cleaning and draping the Submucous fibromyoma 1 3.6
parts. Maximum time taken was 30 minutes, these were (Fig. 1)
the patients, where other concomitant surgical procedure II Atrophic endometrium 1 3.6
Normal finding
4
14.3
had to be carried out along with the hysteroscopy.
Sixty patients where hysteroscopy was carried under Table 3: Various hysteroscopy findings in group ll (infertility)
pethidine + phenargan, were observed in the hospital for (n = 15)
4 hours. Those where general anesthesia was given were Sl. no. observations No. of cases Percentage
kept in the hospital for a duration of 24 hours. Patients were A Hysteroscopic observation
called to attend the oPD after an interval which depen ded (i) Abnormal findings 12 80
upon case to case and further treatment planned. Tubercular endometritis 1 6.7
Various indications for hysteroscopy are shown in Leiomyoma uterus 1 6.7
Table 1. The common indication was DUB (40.50%), other Blocked tubal ostia 10 66.7
indications for hysteroscopy were infertility (21.70%), (ii) Normal findings 3 20
Postmenopausal bleeding (11.60%), suspected leiomyoma B Histopath observation
(11.60%), Lost IUCD with irregular bleeding (07.30%) and – Proliferative endometrium 1 6.7
secondary amenorrhea (07.30%). – Secretory endometrium 14 93.3
In group 1 (DUB) 24 patient (85.71%) out of 28 had C Diagnostic laparoscopy
abnormal hysteroscopic finding (Table 1). Various patho- observation 7 77.7
logical hysteroscopic findings observed in 28 patients is – Blocked tubes
shown below (Table 2). – Patent tubes 2 22.3
130