Page 34 - World Journal of Laparoscopic Surgery
P. 34
Sameer AlOsaimi et al
diSCuSSiOn for CP. Pelvic adhesions following previous pelvic opera-
tion or infection also contribute to a high incidence of
The CP may occur as a result of direct mechanical pene- 9,18
tration with the instrument tip, sharp flexion of the sigmoid perforation. Some authors have also suggested
colonoscope over distended bowel or due to thermal or that patients with multiple comorbidities are at greater
16,19
electrical injury during therapeutic intervention, such risk of perforation. Furthermore, that advanced age of
as polypectomy. patients and endoscopy performed by a trainee shown to
16,20
15
Anderson et al discussed the risks of perforation increase the risk of CP. It was found that mechanical
after either sigmoidoscopy or colonoscopy. The study stress is the most common mechanism of perforation,
compared 10486 colonoscopies with 49501 sigmoido- the other perforations were associated with cone biopsy,
scopies done over 10 years (1987-1996) at Mayo Clinic, electrocautery and pneumatic causes. 21
13,14
they found two deaths secondary to perforation from Similar to the first reported case, we think scoliosis
colonoscopy, corresponding to an overall mortality rate with sever skeletal deformity can interfere with the usual
after a colonoscopy of 0.02% and an incidence of death path of introducing the colonoscope, thus causing CP.
after a perforation of 10%. Colonoscopic perforations may be managed opera-
16
Gatto et al explored a large population-based data- tively or nonoperatively. Several large series have
base to compare the incidence of perforation asso ciated reported that many patients with perforations may be
with both of these flexible endoscopic procedures and treated successfully without operations. Conservative
to investigate what factors predict the occurrence of this treatment includes bowel rest, intravenous fluids, and
complication, they found that the risk of perforation antibiotics to allow the perforation to seal. 15,22-25
after colonoscopy was statistically significantly increased In Korean study, it is reported that 36% of the patients
among patients with diverticulosis and obstruction, were managed conservatively. Nine patients under-
whereas the risk of perforation after sigmoidoscopy was went endoscopic perforation closure using hemoclips.
increased among patients with diverticulosis and abdo- Twenty-nine percent of those patients underwent colonic
minal pain. In their study, there were 77 perforations after resection with anastomosis. In a retrospective review
39286 colonoscopies and 31 perforations after 35298 sig- of laparoscopic repair of colonic perforations, the mean
moidoscopies procedures. Further more, risk of CP from colonic perforation size was 2.7 cm. 26
either procedure increased in association with increasing Operative treatment is most often necessary in
age and the presence of two or more comorbidities. patients with generalized peritonitis, large injuries, or
17
Lohsiriwat et al prospectively reviewed 10124 failed conservative treatment. 27
patients undergoing either colonoscopy or flexible sig- In our case, the perforation located at the anterior
moidoscopy between January 2005 and July 2008. Over wall of sigmoid colon, the patient was in peritonitis, with
a 3.5-year period, there were 15 colonic perforations, radiological evidence of viscus perforation, so surgical
they found that patient gender, emergency endoscopy, intervention was required. As she was hemodynamically
anesthetic method, and the specialty or experience of stable, we chose diagnostic laparoscopy to diagnose and
the endoscopist were not significantly predictive of CP proceed with surgical management.
rate. In the other hand, patient age of over 75 years and The specific operative procedures used will depend
therapeutic colonoscopy were two important risk factors on the size of perforation, the degree of peritoneal soilage,
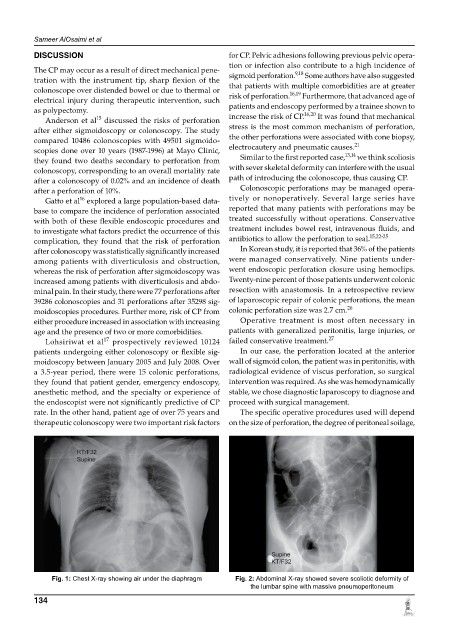
Fig. 1: Chest X-ray showing air under the diaphragm Fig. 2: Abdominal X-ray showed severe scoliotic deformity of
the lumbar spine with massive pneumoperitoneum
134