Page 33 - Laparoscopic Journal - WJOLS
P. 33
WJOLS
A Comparative Study of Single Incision vs Conventional Four Incision Laparoscopic Cholecystectomy
RESuLTS patients was 45.9 ± 9 to 85 years for both groups (Table
2). The average age for those who had SILC was 46.7 ±
Of the 150 patients who had LC at the institute of mini 15 while that for those who had 4PLC was 45.2 ± 14. The
mal access, metabolic and bariatric surgery, Sir Ganga number of males who had SILC was 26 (43.3%), while
Ram Hospital, New Delhi, 61 (50.4%) had conventional
four port laparoscopic cholecystectomy (4PLC), while 34 (56.7%) were females. Those who had conventional 4PLC
had 31 (50.8%) males and 34 (56.7%) females. Indications
60 (49.6%) had SILC (Table 1). The average age of the
for the operation were similar for the two groups (Table 3).
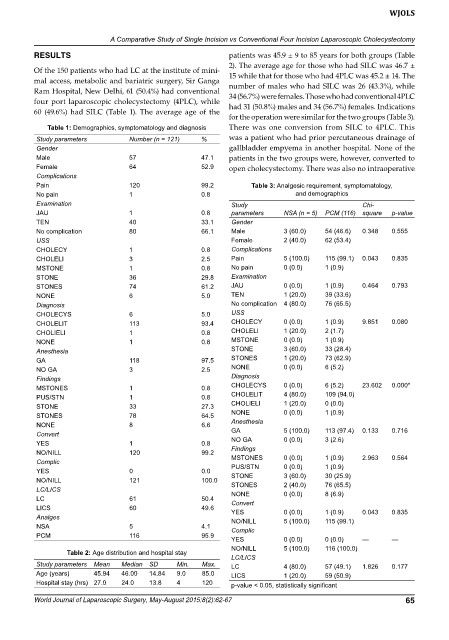
Table 1: Demographics, symptomatology and diagnosis There was one conversion from SILC to 4PLC. This
Study parameters Number (n = 121) % was a patient who had prior percutaneous drainage of
Gender gallbladder empyema in another hospital. None of the
male 57 47.1 patients in the two groups were, however, converted to
Female 64 52.9 open cholecystectomy. There was also no intraoperative
Complications
Pain 120 99.2 Table 3: Analgesic requirement, symptomatology,
No pain 1 0.8 and demographics
Examination Study Chi-
JAU 1 0.8 parameters NSA (n = 5) PCM (116) square p-value
TEN 40 33.1 Gender
No complication 80 66.1 male 3 (60.0) 54 (46.6) 0.348 0.555
USS Female 2 (40.0) 62 (53.4)
CHOLECY 1 0.8 Complications
CHOLELI 3 2.5 Pain 5 (100.0) 115 (99.1) 0.043 0.835
mSTONE 1 0.8 No pain 0 (0.0) 1 (0.9)
STONE 36 29.8 Examination
STONES 74 61.2 JAU 0 (0.0) 1 (0.9) 0.464 0.793
NONE 6 5.0 TEN 1 (20.0) 39 (33.6)
Diagnosis No complication 4 (80.0) 76 (65.5)
CHOLECYS 6 5.0 USS
CHOLELIT 113 93.4 CHOLECY 0 (0.0) 1 (0.9) 9.851 0.080
CHOLIELI 1 0.8 CHOLELI 1 (20.0) 2 (1.7)
NONE 1 0.8 mSTONE 0 (0.0) 1 (0.9)
Anesthesia STONE 3 (60.0) 33 (28.4)
GA 118 97.5 STONES 1 (20.0) 73 (62.9)
NO GA 3 2.5 NONE 0 (0.0) 6 (5.2)
Findings Diagnosis
mSTONES 1 0.8 CHOLECYS 0 (0.0) 6 (5.2) 23.602 0.000*
PUS/STN 1 0.8 CHOLELIT 4 (80.0) 109 (94.0)
STONE 33 27.3 CHOLIELI 1 (20.0) 0 (0.0)
STONES 78 64.5 NONE 0 (0.0) 1 (0.9)
NONE 8 6.6 Anesthesia
Convert GA 5 (100.0) 113 (97.4) 0.133 0.716
YES 1 0.8 NO GA 0 (0.0) 3 (2.6)
NO/NILL 120 99.2 Findings 0 (0.0) 1 (0.9) 2.963 0.564
mSTONES
Complic PUS/STN 0 (0.0) 1 (0.9)
YES 0 0.0 STONE 3 (60.0) 30 (25.9)
NO/NILL 121 100.0 STONES 2 (40.0) 76 (65.5)
LC/LICS NONE 0 (0.0) 8 (6.9)
LC 61 50.4 Convert
LICS 60 49.6 YES 0 (0.0) 1 (0.9) 0.043 0.835
Analges NO/NILL 5 (100.0) 115 (99.1)
NSA 5 4.1 Complic
PCm 116 95.9
YES 0 (0.0) 0 (0.0) — —
NO/NILL 5 (100.0) 116 (100.0)
Table 2: Age distribution and hospital stay
LC/LICS
Study parameters Mean Median SD Min. Max. LC 4 (80.0) 57 (49.1) 1.826 0.177
Age (years) 45.94 46.00 14.84 9.0 85.0 LICS 1 (20.0) 59 (50.9)
Hospital stay (hrs) 27.0 24.0 13.8 4 120 p-value < 0.05, statistically significant
World Journal of Laparoscopic Surgery, May-August 2015;8(2):62-67 65