Page 47 - Journal of Laparoscopic Surgery - WALS Journal
P. 47
WJOLS
Retrorectal Schwannoma
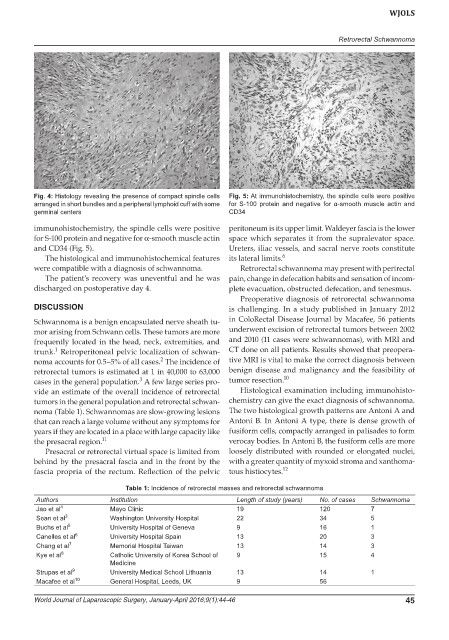
Fig. 4: Histology revealing the presence of compact spindle cells Fig. 5: At immunohistochemistry, the spindle cells were positive
arranged in short bundles and a peripheral lymphoid cuff with some for S-100 protein and negative for α-smooth muscle actin and
germinal centers CD34
immunohistochemistry, the spindle cells were positive peritoneum is its upper limit. Waldeyer fascia is the lower
for S-100 protein and negative for α-smooth muscle actin space which separates it from the supralevator space.
and CD34 (Fig. 5). Ureters, iliac vessels, and sacral nerve roots constitute
The histological and immunohistochemical features its lateral limits. 6
were compatible with a diagnosis of schwannoma. Retrorectal schwannoma may present with perirectal
The patient’s recovery was uneventful and he was pain, change in defecation habits and sensation of incom-
discharged on postoperative day 4. plete evacuation, obstructed defecation, and tenesmus.
Preoperative diagnosis of retrorectal schwannoma
DISCUSSION is challenging. In a study published in January 2012
Schwannoma is a benign encapsulated nerve sheath tu- in ColoRectal Disease Journal by Macafee, 56 patients
mor arising from Schwann cells. These tumors are more underwent excision of retrorectal tumors between 2002
frequently located in the head, neck, extremities, and and 2010 (11 cases were schwannomas), with MRI and
1
trunk. Retroperitoneal pelvic localization of schwan- CT done on all patients. Results showed that preopera-
2
noma accounts for 0.5–5% of all cases. The incidence of tive MRI is vital to make the correct diagnosis between
retrorectal tumors is estimated at 1 in 40,000 to 63,000 benign disease and malignancy and the feasibility of
3
cases in the general population. A few large series pro- tumor resection. 10
vide an estimate of the overall incidence of retrorectal Histological examination including immunohisto-
tumors in the general population and retrorectal schwan- chemistry can give the exact diagnosis of schwannoma.
noma (Table 1). Schwannomas are slow-growing lesions The two histological growth patterns are Antoni A and
that can reach a large volume without any symptoms for Antoni B. In Antoni A type, there is dense growth of
years if they are located in a place with large capacity like fusiform cells, compactly arranged in palisades to form
the presacral region. 11 verocay bodies. In Antoni B, the fusiform cells are more
Presacral or retrorectal virtual space is limited from loosely distributed with rounded or elongated nuclei,
behind by the presacral fascia and in the front by the with a greater quantity of myxoid stroma and xanthoma-
fascia propria of the rectum. Reflection of the pelvic tous histiocytes. 12
Table 1: Incidence of retrorectal masses and retrorectal schwannoma
Authors Institution Length of study (years) No. of cases Schwannoma
Jao et al 4 Mayo Clinic 19 120 7
Sean et al 3 Washington University Hospital 22 34 5
Buchs et al 5 University Hospital of Geneva 9 16 1
Canelles et al 6 University Hospital Spain 13 20 3
Chang et al 7 Memorial Hospital Taiwan 13 14 3
Kye et al 8 Catholic University of Korea School of 9 15 4
Medicine
Strupas et al 9 University Medical School Lithuania 13 14 1
Macafee et al 10 General Hospital, Leeds, UK 9 56
World Journal of Laparoscopic Surgery, January-April 2016;9(1):44-46 45