Page 44 - Journal of Laparoscopic Surgery - WALS Journal
P. 44
Vijaykumar C Bada, Rajvilas Anil Narkhede
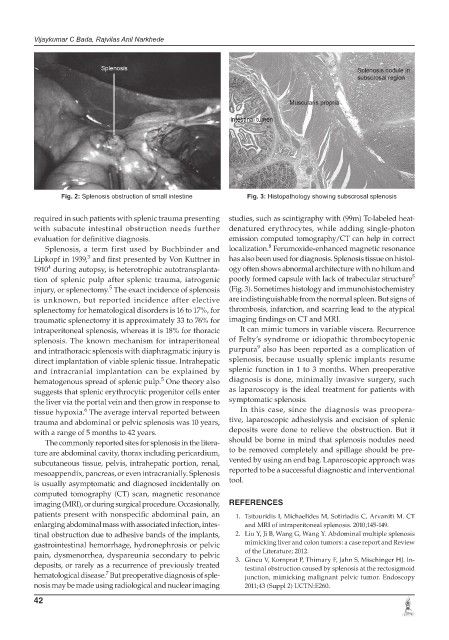
Fig. 2: Splenosis obstruction of small intestine Fig. 3: Histopathology showing subscrosal splenosis
required in such patients with splenic trauma presenting studies, such as scintigraphy with (99m) Tc-labeled heat-
with subacute intestinal obstruction needs further denatured erythrocytes, while adding single-photon
evaluation for definitive diagnosis. emission computed tomography/CT can help in correct
8
Splenosis, a term first used by Buchbinder and localization. Ferumoxide-enhanced magnetic resonance
3
Lipkopf in 1939, and first presented by Von Kuttner in has also been used for diagnosis. Splenosis tissue on histol-
4
1910 during autopsy, is heterotrophic autotransplanta- ogy often shows abnormal architecture with no hilum and
5
tion of splenic pulp after splenic trauma, iatrogenic poorly formed capsule with lack of trabecular structure
5
injury, or splenectomy. The exact incidence of splenosis (Fig. 3). Sometimes histology and immunohistochemistry
is unknown, but reported incidence after elective are indistinguishable from the normal spleen. But signs of
splenectomy for hematological disorders is 16 to 17%, for thrombosis, infarction, and scarring lead to the atypical
traumatic splenectomy it is approximately 33 to 76% for imaging findings on CT and MRI.
intraperitoneal splenosis, whereas it is 18% for thoracic It can mimic tumors in variable viscera. Recurrence
splenosis. The known mechanism for intraperitoneal of Felty’s syndrome or idiopathic thrombocytopenic
9
and intrathoracic splenosis with diaphragmatic injury is purpura also has been reported as a complication of
direct implantation of viable splenic tissue. Intrahepatic splenosis, because usually splenic implants resume
and intracranial implantation can be explained by splenic function in 1 to 3 months. When preoperative
5
hematogenous spread of splenic pulp. One theory also diagnosis is done, minimally invasive surgery, such
suggests that splenic erythrocytic progenitor cells enter as laparoscopy is the ideal treatment for patients with
the liver via the portal vein and then grow in response to symptomatic splenosis.
6
tissue hypoxia. The average interval reported between In this case, since the diagnosis was preopera-
trauma and abdominal or pelvic splenosis was 10 years, tive, laparoscopic adhesiolysis and excision of splenic
with a range of 5 months to 42 years. deposits were done to relieve the obstruction. But it
The commonly reported sites for splenosis in the litera- should be borne in mind that splenosis nodules need
ture are abdominal cavity, thorax including pericardium, to be removed completely and spillage should be pre-
subcutaneous tissue, pelvis, intrahepatic portion, renal, vented by using an end bag. Laparoscopic approach was
mesoappendix, pancreas, or even intracranially. Splenosis reported to be a successful diagnostic and interventional
is usually asymptomatic and diagnosed incidentally on tool.
computed tomography (CT) scan, magnetic resonance
imaging (MRI), or during surgical procedure. Occasionally, REFERENCES
patients present with nonspecific abdominal pain, an 1. Tsitouridis I, Michaelides M, Sotiriadis C, Arvaniti M. CT
enlarging abdominal mass with associated infection, intes- and MRI of intraperitoneal splenosis. 2010;145-149.
tinal obstruction due to adhesive bands of the implants, 2. Liu Y, Ji B, Wang G, Wang Y. Abdominal multiple splenosis
gastrointestinal hemorrhage, hydronephrosis or pelvic mimicking liver and colon tumors: a case report and Review
pain, dysmenorrhea, dyspareunia secondary to pelvic of the Literature; 2012.
deposits, or rarely as a recurrence of previously treated 3. Gincu V, Kornprat P, Thimary F, Jahn S, Mischinger HJ. In-
testinal obstruction caused by splenosis at the rectosigmoid
7
hematological disease. But preoperative diagnosis of sple- junction, mimicking malignant pelvic tumor. Endoscopy
nosis may be made using radiological and nuclear imaging 2011;43 (Suppl 2) UCTN:E260.
42