Page 28 - wjols
P. 28
CASE REPORT
Laparoscopic Heminephroureterectomy in Infants Weighing
Less Than 10 Kilograms: The Two Peculiar Cases
5
6
3
4
1
2
Marianna Iaquinto , Maria-Grazia Scarpa , Roberto De Castro , Daniela Codrich , Edoardo Guida , Alessia Cerrina ,
7
8
Federica Pederiva , Maria A Lembo , Jurgen Schleef 9
AbstrAct
Aim: We report two peculiar cases of laparoscopic heminephrectomy in infants weighing less than 10 kg with megaureter of nonfunctioning
renal upper pole.
Cases description: A 6-month-old boy, with history of upper pole pyo-hydroureteronephrosis managed by percutaneous nephrostomy, was
affected in the left side; while a 17-month-old girl, with history of abdominal mass then proved to be a giant megaureter of nonfunctioning renal
upper pole, was affected in the right side and she was previously treated for primitive obstructive megaureter (in the lower pole). Laparoscopic
heminephroureterectomy with a transperitoneal approach was performed. Mean length of surgery was 160 minutes. We reported no conversion
to open surgery neither intraoperative bleeding/urine leakage. Mean hospitalization duration was 5 days. The reoperation rate was 0%. In both
cases at preliminary follow-up, we reported a good outcome.
Conclusion: Laparoscopic heminephrectomy is considered a technically challenging procedure, especially for small infant but, according to our
experience, it is safe and effective if performed in pediatric centers with high experience in minimally invasive surgery.
Keywords: Heminephrectomy, Infant weighing less than 10 kg, Laparoscopy, Megaureter.
World Journal of Laparoscopic Surgery (2020): 10.5005/jp-journals-10033-1410
bAckground 1,2,4–9 Department of Urologic and Pediatric Surgery, Burlo Garofolo
Nowadays, minimally invasive surgery (MIS) is increasingly used, Children’s Hospital, Trieste, Friuli Venezia Giulia, Italy
compared to open procedures, especially in pediatric urology. 1–4 3 Department of Urologic and Pediatric Surgery, Prof Petrucciani Clinic,
Nevertheless, few reports exist regarding the experience in infants Lecce, Italy
under 2 years old or weighing less than 10 kg, particularly at risk of Corresponding Author: Marianna Iaquinto, Department of Urologic
conversion and/or complications. 5–9 We report two peculiar cases of and Pediatric Surgery, Burlo Garofolo Children’s Hospital, Trieste, Friuli
laparoscopic heminephroureterectomy in infants of this risk group Venezia Giulia, Italy, Phone: +34 594747401, e-mail: i.marianna@
with megaureter of nonfunctioning renal upper pole. hotmail.it
How to cite this article: Iaquinto M, Scarpa M-G, De Castro R, et al.
cAse descriptions Laparoscopic Heminephroureterectomy in Infants Weighing Less Than
10 Kilograms: The Two Peculiar Cases. World J Lap Surg 2020;13(2):80–83.
Case 1 Source of support: Nil
A male infant with prenatal diagnosis of moderate left Conflict of interest: None
hydroureteronephrosis and suspicion the of duplex renal system
(DRS). At birth, the echography confirmed the presence of left DRS
with upper pole (UP) hydroureteronephrosis; he was followed by
nephrologists with ultrasound (US) controls, always stables, and
voiding cystourethrography (VCUG) at 4-month-old, showing the
absence of vesicoureteral reflux (VUR). He was asymptomatic until
the age of 5 months, when he came to the hospital emergency with
high fever and inappetence. Left UP pyohydroureteronephrosis
was diagnosed (Fig. 1), managed by percutaneous nephrostomy
placement and intravenous antibiotic therapy. During the recovery,
a descending pyelography was performed by the nephrostomy
that showed no passage of contrast into the bladder (Fig. 2). After
1 month, a dynamic renal scan (Mag3) was performed: bilateral
DRS with ectopic megaureter (MU) in left nonfunctioning UP was
described.
Case 2
A female infant with prenatal diagnosis of severe
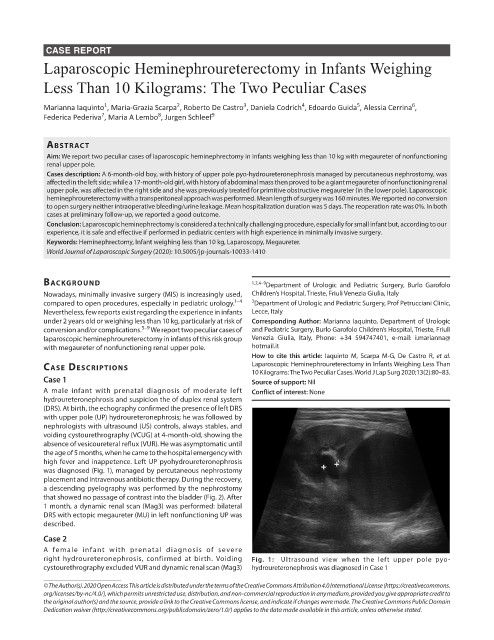
right hydroureteronephrosis, confirmed at birth. Voiding Fig. 1: Ultrasound view when the left upper pole pyo-
cystourethrography excluded VUR and dynamic renal scan (Mag3) hydroureteronephrosis was diagnosed in Case 1
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.
org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to
the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain
Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.