Page 22 - wjols
P. 22
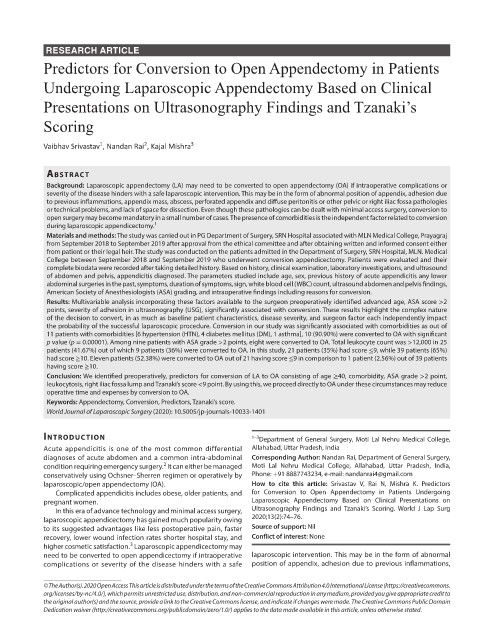
RESEARCH ARTICLE
Predictors for Conversion to Open Appendectomy in Patients
Undergoing Laparoscopic Appendectomy Based on Clinical
Presentations on Ultrasonography Findings and Tzanaki’s
Scoring
1
2
Vaibhav Srivastav , Nandan Rai , Kajal Mishra 3
AbstrAct
Background: Laparoscopic appendectomy (LA) may need to be converted to open appendectomy (OA) if intraoperative complications or
severity of the disease hinders with a safe laparoscopic intervention. This may be in the form of abnormal position of appendix, adhesion due
to previous inflammations, appendix mass, abscess, perforated appendix and diffuse peritonitis or other pelvic or right iliac fossa pathologies
or technical problems, and lack of space for dissection. Even though these pathologies can be dealt with minimal access surgery, conversion to
open surgery may become mandatory in a small number of cases. The presence of comorbidities is the independent factor related to conversion
during laparoscopic appendicectomy. 1
Materials and methods: The study was carried out in PG Department of Surgery, SRN Hospital associated with MLN Medical College, Prayagraj
from September 2018 to September 2019 after approval from the ethical committee and after obtaining written and informed consent either
from patient or their legal heir. The study was conducted on the patients admitted in the Department of Surgery, SRN Hospital, MLN. Medical
College between September 2018 and September 2019 who underwent conversion appendicectomy. Patients were evaluated and their
complete biodata were recorded after taking detailed history. Based on history, clinical examination, laboratory investigations, and ultrasound
of abdomen and pelvis, appendicitis diagnosed. The parameters studied include age, sex, previous history of acute appendicitis any lower
abdominal surgeries in the past, symptoms, duration of symptoms, sign, white blood cell (WBC) count, ultrasound abdomen and pelvis findings,
American Society of Anesthesiologists (ASA) grading, and intraoperative findings including reasons for conversion.
Results: Multivariable analysis incorporating these factors available to the surgeon preoperatively identified advanced age, ASA score >2
points, severity of adhesion in ultrasonography (USG), significantly associated with conversion. These results highlight the complex nature
of the decision to convert, in as much as baseline patient characteristics, disease severity, and surgeon factor each independently impact
the probability of the successful laparoscopic procedure. Conversion in our study was significantly associated with comorbidities as out of
11 patients with comorbidities [6 hypertension (HTN), 4 diabetes mellitus (DM), 1 asthma], 10 (90.90%) were converted to OA with significant
p value (p = 0.00001). Among nine patients with ASA grade >2 points, eight were converted to OA. Total leukocyte count was >12,000 in 25
patients (41.67%) out of which 9 patients (36%) were converted to OA. In this study, 21 patients (35%) had score ≤9, while 39 patients (65%)
had score ≥10. Eleven patients (52.38%) were converted to OA out of 21 having score ≤9 in comparison to 1 patient (2.56%) out of 39 patients
having score ≥10.
Conclusion: We identified preoperatively, predictors for conversion of LA to OA consisting of age ≥40, comorbidity, ASA grade >2 point,
leukocytosis, right iliac fossa lump and Tzanaki’s score <9 point. By using this, we proceed directly to OA under these circumstances may reduce
operative time and expenses by conversion to OA.
Keywords: Appendectomy, Conversion, Predictors, Tzanaki’s score.
World Journal of Laparoscopic Surgery (2020): 10.5005/jp-journals-10033-1401
IntroductIon 1–3 Department of General Surgery, Moti Lal Nehru Medical College,
Acute appendicitis is one of the most common differential Allahabad, Uttar Pradesh, India
diagnoses of acute abdomen and a common intra-abdominal Corresponding Author: Nandan Rai, Department of General Surgery,
2
condition requiring emergency surgery. It can either be managed Moti Lal Nehru Medical College, Allahabad, Uttar Pradesh, India,
conservatively using Ochsner–Sherren regimen or operatively by Phone: +91 8887743234, e-mail: nandanrai4@gmail.com
laparoscopic/open appendectomy (OA). How to cite this article: Srivastav V, Rai N, Mishra K. Predictors
Complicated appendicitis includes obese, older patients, and for Conversion to Open Appendectomy in Patients Undergoing
pregnant women. Laparoscopic Appendectomy Based on Clinical Presentations on
In this era of advance technology and minimal access surgery, Ultrasonography Findings and Tzanaki’s Scoring. World J Lap Surg
laparoscopic appendicectomy has gained much popularity owing 2020;13(2):74–76.
to its suggested advantages like less postoperative pain, faster Source of support: Nil
recovery, lower wound infection rates shorter hospital stay, and Conflict of interest: None
3
higher cosmetic satisfaction. Laparoscopic appendicectomy may
need to be converted to open appendicectomy if intraoperative laparoscopic intervention. This may be in the form of abnormal
complications or severity of the disease hinders with a safe position of appendix, adhesion due to previous inflammations,
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.
org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to
the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain
Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.