Page 20 - wjols
P. 20
Comparison Objective Structured Assessment of Camera Navigation Skills Score—Pre- and Post-training Intervention
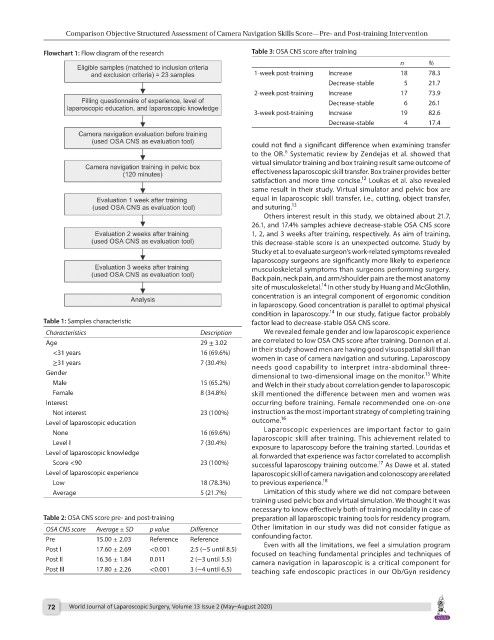
Flowchart 1: Flow diagram of the research Table 3: OSA CNS score after training
n %
1-week post-training Increase 18 78.3
Decrease-stable 5 21.7
2-week post-training Increase 17 73.9
Decrease-stable 6 26.1
3-week post-training Increase 19 82.6
Decrease-stable 4 17.4
could not find a significant difference when examining transfer
6
to the OR. Systematic review by Zendejas et al. showed that
virtual simulator training and box training result same outcome of
effectiveness laparoscopic skill transfer. Box trainer provides better
12
satisfaction and more time concise. Loukas et al. also revealed
same result in their study. Virtual simulator and pelvic box are
equal in laparoscopic skill transfer, i.e., cutting, object transfer,
and suturing. 13
Others interest result in this study, we obtained about 21.7,
26.1, and 17.4% samples achieve decrease-stable OSA CNS score
1, 2, and 3 weeks after training, respectively. As aim of training,
this decrease-stable score is an unexpected outcome. Study by
Stucky et al. to evaluate surgeon’s work-related symptoms revealed
laparoscopy surgeons are significantly more likely to experience
musculoskeletal symptoms than surgeons performing surgery.
Back pain, neck pain, and arm/shoulder pain are the most anatomy
14
site of musculoskeletal. In other study by Huang and McGlothlin,
concentration is an integral component of ergonomic condition
in laparoscopy. Good concentration is parallel to optimal physical
14
condition in laparoscopy. In our study, fatigue factor probably
Table 1: Samples characteristic factor lead to decrease-stable OSA CNS score.
Characteristics Description We revealed female gender and low laparoscopic experience
Age 29 ± 3.02 are correlated to low OSA CNS score after training. Donnon et al.
<31 years 16 (69.6%) in their study showed men are having good visuospatial skill than
≥31 years 7 (30.4%) women in case of camera navigation and suturing. Laparoscopy
needs good capability to interpret intra-abdominal three-
Gender dimensional to two-dimensional image on the monitor. White
15
Male 15 (65.2%) and Welch in their study about correlation gender to laparoscopic
Female 8 (34.8%) skill mentioned the difference between men and women was
Interest occurring before training. Female recommended one-on-one
Not interest 23 (100%) instruction as the most important strategy of completing training
Level of laparoscopic education outcome. 16
None 16 (69.6%) Laparoscopic experiences are important factor to gain
Level I 7 (30.4%) laparoscopic skill after training. This achievement related to
exposure to laparoscopy before the training started. Louridas et
Level of laparoscopic knowledge al. forwarded that experience was factor correlated to accomplish
Score <90 23 (100%) successful laparoscopy training outcome. As Dawe et al. stated
17
Level of laparoscopic experience laparoscopic skill of camera navigation and colonoscopy are related
Low 18 (78.3%) to previous experience. 18
Average 5 (21.7%) Limitation of this study where we did not compare between
training used pelvic box and virtual simulation. We thought it was
necessary to know effectively both of training modality in case of
Table 2: OSA CNS score pre- and post-training preparation all laparoscopic training tools for residency program.
OSA CNS score Average ± SD p value Difference Other limitation in our study was did not consider fatigue as
Pre 15.00 ± 2.03 Reference Reference confounding factor.
Even with all the limitations, we feel a simulation program
Post I 17.60 ± 2.69 <0.001 2.5 (−5 until 8.5) focused on teaching fundamental principles and techniques of
Post II 16.36 ± 1.84 0.011 2 (−3 until 5.5) camera navigation in laparoscopic is a critical component for
Post III 17.80 ± 2.26 <0.001 3 (−4 until 6.5) teaching safe endoscopic practices in our Ob/Gyn residency
72 World Journal of Laparoscopic Surgery, Volume 13 Issue 2 (May–August 2020)