Page 21 - wjols
P. 21
Comparison Objective Structured Assessment of Camera Navigation Skills Score—Pre- and Post-training Intervention
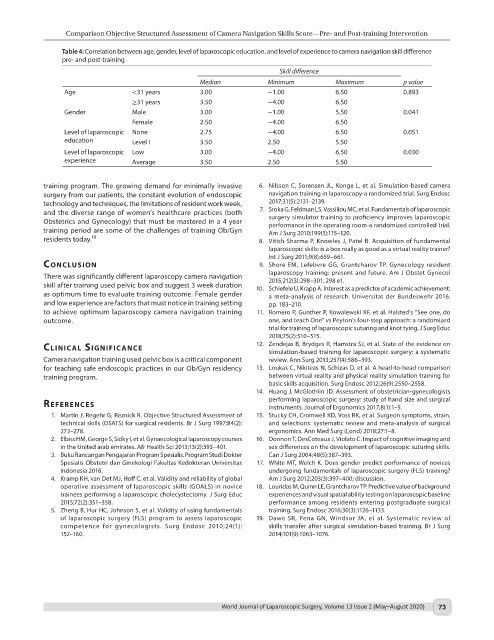
Table 4: Correlation between age, gender, level of laparoscopic education, and level of experience to camera navigation skill difference
pre- and post-training
Skill difference
Median Minimum Maximum p value
Age <31 years 3.00 −1.00 6.50 0.893
≥31 years 3.50 −4.00 6.50
Gender Male 3.00 −1.00 5.50 0.041
Female 2.50 −4.00 6.50
Level of laparoscopic None 2.75 −4.00 6.50 0.051
education Level I 3.50 2.50 5.50
Level of laparoscopic Low 3.00 −4.00 6.50 0.030
experience Average 3.50 2.50 5.50
training program. The growing demand for minimally invasive 6. Nilsson C, Sorensen JL, Konge L, et al. Simulation-based camera
surgery from our patients, the constant evolution of endoscopic navigation training in laparoscopy-a randomized trial. Surg Endosc
technology and techniques, the limitations of resident work week, 2017;31(5):2131–2139.
and the diverse range of women’s healthcare practices (both 7. Sroka G, Feldman LS, Vassiliou MC, et al. Fundamentals of laparoscopic
Obstetrics and Gynecology) that must be mastered in a 4 year surgery simulator training to proficiency improves laparoscopic
training period are some of the challenges of training Ob/Gyn performance in the operating room-a randomized controlled trial.
Am J Surg 2010;199(1):115–120.
residents today. 19 8. Vitish-Sharma P, Knowles J, Patel B. Acquisition of fundamental
laparoscopic skills: is a box really as good as a virtual reality trainer?
Int J Surg 2011;9(8):659–661.
conclusIon 9. Shore EM, Lefebvre GG, Grantcharov TP. Gynecology resident
There was significantly different laparoscopy camera navigation laparoscopy training: present and future. Am J Obstet Gynecol
2015;212(3):298–301, 298 e1.
skill after training used pelvic box and suggest 3 week duration 10. Schiefele U, Krapp A. Interest as a predictor of academic achievement:
as optimum time to evaluate training outcome. Female gender a meta-analysis of research. Universitat der Bundeswehr 2016.
and low experience are factors that must notice in training setting pp. 183–210.
to achieve optimum laparoscopy camera navigation training 11. Romero P, Gunther P, Kowalewski KF, et al. Halsted’s “See one, do
outcome. one, and teach One” vs Peyton’s four-step approach: a randomized
trial for training of laparoscopic suturing and knot tying. J Surg Educ
2018;75(2):510–515.
clInIcAl sIgnIfIcAnce 12. Zendejas B, Brydges R, Hamstra SJ, et al. State of the evidence on
simulation-based training for laparoscopic surgery: a systematic
Camera navigation training used pelvic box is a critical component review. Ann Surg 2013;257(4):586–593.
for teaching safe endoscopic practices in our Ob/Gyn residency 13. Loukas C, Nikiteas N, Schizas D, et al. A head-to-head comparison
training program. between virtual reality and physical reality simulation training for
basic skills acquisition. Surg Endosc 2012;26(9):2550–2558.
14. Huang J, McGlothlin JD. Assessment of obstetrician-gynecologists
performing laparoscopic surgery: study of hand size and surgical
references instruments. Journal of Ergonomics 2017;8(1):1–5.
1. Martin J, Regehr G, Reznick R. Objective Structured Assessment of 15. Stucky CH, Cromwell KD, Voss RK, et al. Surgeon symptoms, strain,
technical skills (OSATS) for surgical residents. Br J Surg 1997;84(2): and selections: systematic review and meta-analysis of surgical
273–278. ergonomics. Ann Med Surg (Lond) 2018;27:1–8.
2. Elbiss HM, George S, Sidky I, et al. Gynaecological laparoscopy courses 16. Donnon T, DesCoteaux J, Violato C. Impact of cognitive imaging and
in the United arab emirates. Afr Health Sci 2013;13(2):393–401. sex differences on the development of laparoscopic suturing skills.
3. Buku Rancangan Pengajaran Program Spesialis. Program Studi Dokter Can J Surg 2004;48(5):387–393.
Spesialis Obstetri dan Ginekologi Fakultas Kedokteran Universitas 17. White MT, Welch K. Does gender predict performance of novices
Indonesia 2016. undergoing fundamentals of laparoscopic surgery (FLS) training?
4. Kramp KH, van Det MJ, Hoff C, et al. Validity and reliability of global Am J Surg 2012;203(3):397–400; discussion.
operative assessment of laparoscopic skills (GOALS) in novice 18. Louridas M, Quinn LE, Grantcharov TP. Predictive value of background
trainees performing a laparoscopic cholecystectomy. J Surg Educ experiences and visual spatial ability testing on laparoscopic baseline
2015;72(2):351–358. performance among residents entering postgraduate surgical
5. Zheng B, Hur HC, Johnson S, et al. Validity of using fundamentals training. Surg Endosc 2016;30(3):1126–1133.
of laparoscopic surgery (FLS) program to assess laparoscopic 19. Dawe SR, Pena GN, Windsor JA, et al. Systematic review of
competence for gynecologists. Surg Endosc 2010;24(1): skills transfer after surgical simulation-based training. Br J Surg
152–160. 2014;101(9):1063–1076.
World Journal of Laparoscopic Surgery, Volume 13 Issue 2 (May–August 2020) 73