Page 32 - World Journal of Laparoscopic Surgeons
P. 32
WJOLS
Posterior Rectus Sheath
A B
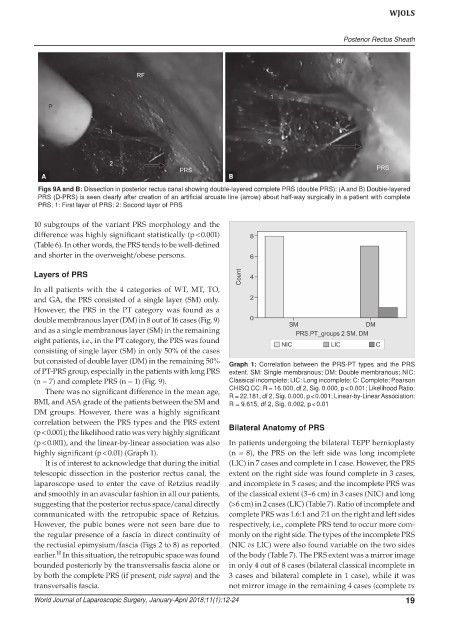
Figs 9A and B: Dissection in posterior rectus canal showing double-layered complete PRS (double PRS): (A and B) Double-layered
PRS (D-PRS) is seen clearly after creation of an artificial arcuate line (arrow) about half-way surgically in a patient with complete
PRS; 1: First layer of PRS; 2: Second layer of PRS
10 subgroups of the variant PRS morphology and the
difference was highly significant statistically (p < 0.001)
(Table 6). In other words, the PRS tends to be well-defined
and shorter in the overweight/obese persons.
Layers of PRS
In all patients with the 4 categories of WT, MT, TO,
and GA, the PRS consisted of a single layer (SM) only.
However, the PRS in the PT category was found as a
double membranous layer (DM) in 8 out of 16 cases (Fig. 9)
and as a single membranous layer (SM) in the remaining
eight patients, i.e., in the PT category, the PRS was found
consisting of single layer (SM) in only 50% of the cases
but consisted of double layer (DM) in the remaining 50% Graph 1: Correlation between the PRS-PT types and the PRS
of PT-PRS group, especially in the patients with long PRS extent. SM: Single membranous; DM: Double membranous; NIC:
(n = 7) and complete PRS (n = 1) (Fig. 9). Classical incomplete; LIC: Long incomplete; C: Complete; Pearson
There was no significant difference in the mean age, CHISQ CC: R = 16.000, df 2, Sig. 0.000, p < 0.001; Likelihood Ratio:
R = 22.181, df 2, Sig. 0.000, p < 0.001; Linear-by-Linear Association:
BMI, and ASA grade of the patients between the SM and R = 9.615, df 2, Sig. 0.002, p < 0.01
DM groups. However, there was a highly significant
correlation between the PRS types and the PRS extent
(p < 0.001); the likelihood ratio was very highly significant Bilateral Anatomy of PRS
(p < 0.001), and the linear-by-linear association was also In patients undergoing the bilateral TEPP hernioplasty
highly significant (p < 0.01) (Graph 1). (n = 8), the PRS on the left side was long incomplete
It is of interest to acknowledge that during the initial (LIC) in 7 cases and complete in 1 case. However, the PRS
telescopic dissection in the posterior rectus canal, the extent on the right side was found complete in 3 cases,
laparoscope used to enter the cave of Retzius readily and incomplete in 5 cases; and the incomplete PRS was
and smoothly in an avascular fashion in all our patients, of the classical extent (3–6 cm) in 3 cases (NIC) and long
suggesting that the posterior rectus space/canal directly (>6 cm) in 2 cases (LIC) (Table 7). Ratio of incomplete and
communicated with the retropubic space of Retzius. complete PRS was 1.6:1 and 7:1 on the right and left sides
However, the pubic bones were not seen bare due to respectively, i.e., complete PRS tend to occur more com-
the regular presence of a fascia in direct continuity of monly on the right side. The types of the incomplete PRS
the rectusial epimysium/fascia (Figs 2 to 8) as reported (NIC vs LIC) were also found variable on the two sides
10
earlier. In this situation, the retropubic space was found of the body (Table 7). The PRS extent was a mirror image
bounded posteriorly by the transversalis fascia alone or in only 4 out of 8 cases (bilateral classical incomplete in
by both the complete PRS (if present, vide supra) and the 3 cases and bilateral complete in 1 case), while it was
transversalis fascia. not mirror image in the remaining 4 cases (complete vs
World Journal of Laparoscopic Surgery, January-April 2018;11(1):12-24 19