Page 70 - World Journal of Laparoscopic Surgery
P. 70
Type VI Choledochal Cyst Diagnosed Intraoperatively
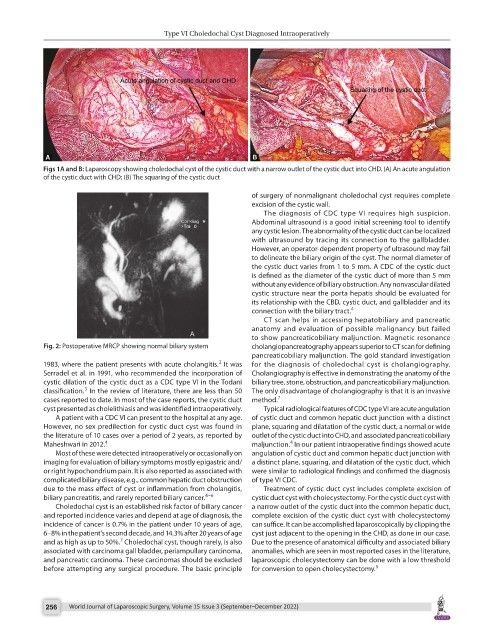
Figs 1A and B: Laparoscopy showing choledochal cyst of the cystic duct with a narrow outlet of the cystic duct into CHD. (A) An acute angulation
of the cystic duct with CHD; (B) The squaring of the cystic duct
of surgery of nonmalignant choledochal cyst requires complete
excision of the cystic wall.
The diagnosis of CDC type VI requires high suspicion.
Abdominal ultrasound is a good initial screening tool to identify
any cystic lesion. The abnormality of the cystic duct can be localized
with ultrasound by tracing its connection to the gallbladder.
However, an operator-dependent property of ultrasound may fail
to delineate the biliary origin of the cyst. The normal diameter of
the cystic duct varies from 1 to 5 mm. A CDC of the cystic duct
is defined as the diameter of the cystic duct of more than 5 mm
without any evidence of biliary obstruction. Any nonvascular dilated
cystic structure near the porta hepatis should be evaluated for
its relationship with the CBD, cystic duct, and gallbladder and its
connection with the biliary tract. 4
CT scan helps in accessing hepatobiliary and pancreatic
anatomy and evaluation of possible malignancy but failed
to show pancreaticobiliary maljunction. Magnetic resonance
Fig. 2: Postoperative MRCP showing normal biliary system cholangiopancreatography appears superior to CT scan for defining
pancreaticobiliary maljunction. The gold standard investigation
2
1983, where the patient presents with acute cholangitis. It was for the diagnosis of choledochal cyst is cholangiography.
Serradel et al. in 1991, who recommended the incorporation of Cholangiography is effective in demonstrating the anatomy of the
cystic dilation of the cystic duct as a CDC type VI in the Todani biliary tree, stone, obstruction, and pancreaticobiliary maljunction.
3
classification. In the review of literature, there are less than 50 The only disadvantage of cholangiography is that it is an invasive
cases reported to date. In most of the case reports, the cystic duct method. 7
cyst presented as cholelithiasis and was identified intraoperatively. Typical radiological features of CDC type VI are acute angulation
A patient with a CDC VI can present to the hospital at any age. of cystic duct and common hepatic duct junction with a distinct
However, no sex predilection for cystic duct cyst was found in plane, squaring and dilatation of the cystic duct, a normal or wide
the literature of 10 cases over a period of 2 years, as reported by outlet of the cystic duct into CHD, and associated pancreaticobiliary
4
Maheshwari in 2012. 4 maljunction. In our patient intraoperative findings showed acute
Most of these were detected intraoperatively or occasionally on angulation of cystic duct and common hepatic duct junction with
imaging for evaluation of biliary symptoms mostly epigastric and/ a distinct plane, squaring, and dilatation of the cystic duct, which
or right hypochondrium pain. It is also reported as associated with were similar to radiological findings and confirmed the diagnosis
complicated biliary disease, e.g., common hepatic duct obstruction of type VI CDC.
due to the mass effect of cyst or inflammation from cholangitis, Treatment of cystic duct cyst includes complete excision of
biliary pancreatitis, and rarely reported biliary cancer. 4–6 cystic duct cyst with cholecystectomy. For the cystic duct cyst with
Choledochal cyst is an established risk factor of biliary cancer a narrow outlet of the cystic duct into the common hepatic duct,
and reported incidence varies and depend at age of diagnosis, the complete excision of the cystic duct cyst with cholecystectomy
incidence of cancer is 0.7% in the patient under 10 years of age, can suffice. It can be accomplished laparoscopically by clipping the
6–8% in the patient’s second decade, and 14.3% after 20 years of age cyst just adjacent to the opening in the CHD, as done in our case.
7
and as high as up to 50%. Choledochal cyst, though rarely, is also Due to the presence of anatomical difficulty and associated biliary
associated with carcinoma gall bladder, periampullary carcinoma, anomalies, which are seen in most reported cases in the literature,
and pancreatic carcinoma. These carcinomas should be excluded laparoscopic cholecystectomy can be done with a low threshold
before attempting any surgical procedure. The basic principle for conversion to open cholecystectomy. 5
256 World Journal of Laparoscopic Surgery, Volume 15 Issue 3 (September–December 2022)