Page 35 - World Journal of Laparoscopic Surgery
P. 35
Hemorrhoidectomy by MIPH
using a transonic circular stapling instrument, introduced by Dr Table 1: Distribution of patients undergoing MIPH
Antonio Longo in the 1990s. 1–4 Diagnosis No. of patients %
Stapled hemorrhoidopexy is a technique that is globally
accepted and widely used. Even though there is chance of Bleeding PR with grade II internal 40 24.1%
recurrence and it is also a costly procedure as compared with hemorrhoids
open methods. The minimally invasive procedure for hemorrhoids Grade III hemorrhoids 52 31.3%
5
or MIPH has made significant strides in the field of proctology. Grade III hemorrhoids 28 16.9%
The principle of this operation is to remove and cut off anal
hemorrhoidal vascular cushion from an area above the dentate Interno-external piles 14 8.4%
line and reposit the anal columns in such a way that the staple line Prolapsed piles 22 13.3%
is above the dentate line. 5,6 Thrombosed piles 10 6.0%
MAterIAls And Methods
It represents an institutional prospective study and included
patients who underwent MIPH operated on 4th January, 2019–6th
December, 2020. Written informed consent was taken from patients
prior to study enrollment. The patients undergoing SH were
followed up through regular visits to the outpatient department
every week for 1 month, every 15 days for the next 2 months, and
up to a period of 6 months post surgery.
Eligibility Criteria
Patients who had undergone MIPH surgery.
Exclusion Criteria
Age less than 18 years, hemorrhoids were associated with any other
anal pathology during surgery.
All clinical data were collected from a standardized questionnaire
evaluation obtained through follow-up. The following variables
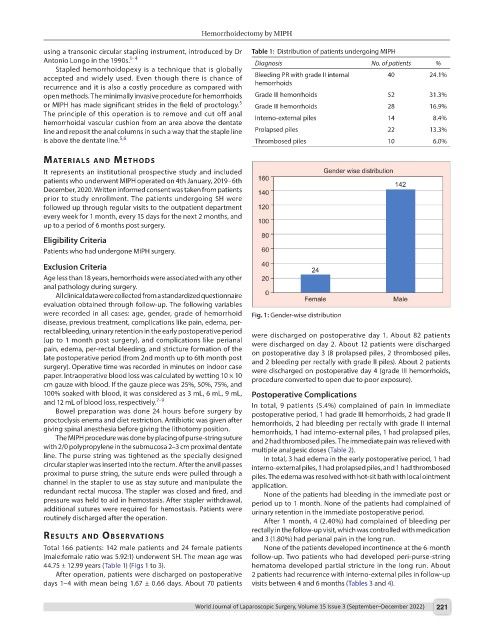
were recorded in all cases: age, gender, grade of hemorrhoid Fig. 1: Gender-wise distribution
disease, previous treatment, complications like pain, edema, per-
rectal bleeding, urinary retention in the early postoperative period were discharged on postoperative day 1. About 82 patients
(up to 1 month post surgery), and complications like perianal were discharged on day 2. About 12 patients were discharged
pain, edema, per-rectal bleeding, and stricture formation of the on postoperative day 3 (8 prolapsed piles, 2 thrombosed piles,
late postoperative period (from 2nd month up to 6th month post and 2 bleeding per rectally with grade II piles). About 2 patients
surgery). Operative time was recorded in minutes on indoor case were discharged on postoperative day 4 (grade III hemorrhoids,
paper. Intraoperative blood loss was calculated by wetting 10 × 10 procedure converted to open due to poor exposure).
cm gauze with blood. If the gauze piece was 25%, 50%, 75%, and
100% soaked with blood, it was considered as 3 mL, 6 mL, 9 mL, Postoperative Complications
and 12 mL of blood loss, respectively. 7–9 In total, 9 patients (5.4%) complained of pain in immediate
Bowel preparation was done 24 hours before surgery by postoperative period, 1 had grade III hemorrhoids, 2 had grade II
proctoclysis enema and diet restriction. Antibiotic was given after hemorrhoids, 2 had bleeding per rectally with grade II internal
giving spinal anesthesia before giving the lithotomy position. hemorrhoids, 1 had interno-external piles, 1 had prolapsed piles,
The MIPH procedure was done by placing of purse-string suture and 2 had thrombosed piles. The immediate pain was relieved with
with 2/0 polypropylene in the submucosa 2–3 cm proximal dentate multiple analgesic doses (Table 2).
line. The purse string was tightened as the specially designed In total, 3 had edema in the early postoperative period, 1 had
circular stapler was inserted into the rectum. After the anvil passes interno-external piles, 1 had prolapsed piles, and 1 had thrombosed
proximal to purse string, the suture ends were pulled through a piles. The edema was resolved with hot-sit bath with local ointment
channel in the stapler to use as stay suture and manipulate the application.
redundant rectal mucosa. The stapler was closed and fired, and None of the patients had bleeding in the immediate post or
pressure was held to aid in hemostasis. After stapler withdrawal, period up to 1 month. None of the patients had complained of
additional sutures were required for hemostasis. Patients were urinary retention in the immediate postoperative period.
routinely discharged after the operation. After 1 month, 4 (2.40%) had complained of bleeding per
rectally in the follow-up visit, which was controlled with medication
results And observAtIons and 3 (1.80%) had perianal pain in the long run.
Total 166 patients: 142 male patients and 24 female patients None of the patients developed incontinence at the 6-month
(male:female ratio was 5.92:1) underwent SH. The mean age was follow-up. Two patients who had developed peri-purse-string
44.75 ± 12.99 years (Table 1) (Figs 1 to 3). hematoma developed partial stricture in the long run. About
After operation, patients were discharged on postoperative 2 patients had recurrence with interno-external piles in follow-up
days 1–4 with mean being 1.67 ± 0.66 days. About 70 patients visits between 4 and 6 months (Tables 3 and 4).
World Journal of Laparoscopic Surgery, Volume 15 Issue 3 (September–December 2022) 221