Page 23 - World Journal of Laparoscopic Surgery
P. 23
Transillumination in Laparoscopic Hernia Repair
that no intestinal, or other tissues is adherent to the back of the wall analyze the outcomes. The identified parameters were compared
which will appear as a dark area in the shining field. Transillumination and the level of significance was set at the 0.05 alpha level. All the
will also localize the course of the blood vessels traversing the results are shown as median (interquartile range).
abdominal wall a proactive step to avoid vascular injuries during
trocar insertion. Once this procedure is completed, the scope’s light results
source is returned back to the optimal intensity. Sixty-two patients were assessed for eligibility. The analysis included
Patients’ Assessment and Outcomes 46 patients for 6 months duration, of whom 23 were randomized to
group I and 23 to group II. No significant differences were present
Assessment of the patients was done at the operation, and a between the two groups regarding patient characteristics or
week; a month; and 3 and 6 months after the surgery. The primary operation times (Table 1). The direct distances between the primary
endpoint was the length of the direct distance between the trocar and the left midaxillary line were significantly less in group I,
primary port and the left midaxillary line. As this distance is inversely median of 35 mm (15–65 mm) than in group II, median of 75 mm
proportional to the distance that will exist between the camera port (45–85 mm) (p = 0.013). There were no significant differences
and the hernial defect, the higher this last distance, the easier it will between the two groups regarding postoperative complications.
be to manipulate the instruments. Secondary outcomes involved There were no complications or hernia recurrence within the
the duration of the operation and adverse events. 6 months follow-up in either group.
Statistical Analysis
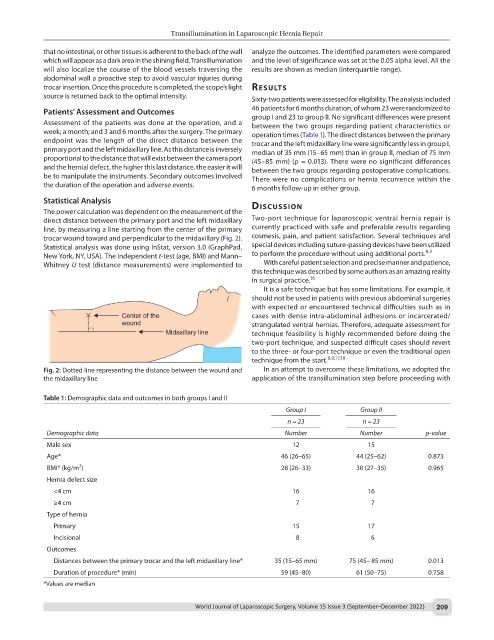
The power calculation was dependent on the measurement of the dIscussIon
direct distance between the primary port and the left midaxillary Two-port technique for laparoscopic ventral hernia repair is
line, by measuring a line starting from the center of the primary currently practiced with safe and preferable results regarding
trocar wound toward and perpendicular to the midaxillary (Fig. 2). cosmesis, pain, and patient satisfaction. Several techniques and
Statistical analysis was done using InStat, version 3.0 (GraphPad, special devices including suture-passing devices have been utilized
New York, NY, USA). The independent t-test (age, BMI) and Mann– to perform the procedure without using additional ports. 8,9
Whitney U test (distance measurements) were implemented to With careful patient selection and precise manner and patience,
this technique was described by some authors as an amazing reality
in surgical practice. 16
It is a safe technique but has some limitations. For example, it
should not be used in patients with previous abdominal surgeries
with expected or encountered technical difficulties such as in
cases with dense intra-abdominal adhesions or incarcerated/
strangulated ventral hernias. Therefore, adequate assessment for
technique feasibility is highly recommended before doing the
two-port technique, and suspected difficult cases should revert
to the three- or four-port technique or even the traditional open
technique from the start. 8,9,17,18
Fig. 2: Dotted line representing the distance between the wound and In an attempt to overcome these limitations, we adopted the
the midaxillary line application of the transillumination step before proceeding with
Table 1: Demographic data and outcomes in both groups I and II
Group I Group II
n = 23 n = 23
Demographic data Number Number p-value
Male sex 12 15
Age* 46 (26–65) 44 (25–62) 0.873
2
BMI* (kg/m ) 28 (26–33) 30 (27–35) 0.965
Hernia defect size
<4 cm 16 16
≥4 cm 7 7
Type of hernia
Primary 15 17
Incisional 8 6
Outcomes
Distances between the primary trocar and the left midaxillary line* 35 (15–65 mm) 75 (45– 85 mm) 0.013
Duration of procedure* (min) 59 (45–80) 61 (50–75) 0.758
*Values are median
World Journal of Laparoscopic Surgery, Volume 15 Issue 3 (September–December 2022) 209