Page 19 - World Journal of Laparoscopic Surgery
P. 19
Anatomical Variations of Rouviere’s Sulcus in Egyptian Patients
dIscussIon
With the increasing number of LCs all over the world, there is a
risk of biliary tract injuries (0.4–1.5% of cases) inspite of marked
improvement in the techniques and devices of laparoscopies. 10
Anatomical variation of the biliary system, together with the
lack of proper identification of the anomalies of the vascular and
biliary structures, are the main causes of iatrogenic injuries of the
biliary tree. 11
Rouviere’s sulcus, also known as incisura hepatica dextra or
Gans incisura, was first described by Henri Rouviere in 1924, as a
cleft 2–3 cm. Just anterior to segment I and running to the right
of the liver hilum and is usually containing the right portal triad,
and it marks the plane of common bile duct accurately. Although
not all the classic anatomical literatures include data on RS, its
importance is due to its location in a line where the cystic duct
and cystic artery lay anterosuperior to the sulcus, and the common
bile duct lays below the level of RS, so the minimal complications
Fig. 6: RS in group A (non-cirrhotic)
occur if the surgeon starts dissection during cholecystectomy in a
plane anterior to it. 4
Table 2: Data collected about the RS in group B
Gans described RS in 80% of the livers, Reynaud et al. reported
RS Number of patients Percentage the incisura dextra of Gans in 73% of cases, Hugh et al. found it in
(A) Sulcus 9 22.5 90% of livers. 12–14
To the best of our knowledge, no research found discussing RS
Open 3
in patients with liver cirrhosis. In this study, we found RS in 92% of
Closed 6 the patients having no cirrhosis while it was found in 50% of the
(B) Scar 11 27.5 patients having liver cirrhosis.
Identification of RS provides an easy landmark for starting
(C) Absent 20 50 dissection of Calot’s triangle for safe LC. In this study, among
the 250 patients RS was clearly identified in 92% of patients; as
a deep sulcus in 76%, as a scar in 16%, while it was absent in the
remaining 8% of patients. These results are comparable to results
of Abhijeet Kumar study in 2020 as they found the sulcus present
in 90.4%; as a sulcus in (77.1%) and scar in (22.9%) but differ from
Stuart Lockhart in 2018 how mentioned that RS, occurs in over
80% and absent in 20% of normal livers during laparoscopic
cholcystectomy. 15,16 This study also differs from the Lazarus,
et al. study in 2018 as their study included the gross anatomical
examination of 75 formalin-fixed, adult livers and not on living
patients the sulcus was present in 82.67% and the study of Rohin
Garg 2019, where the RS was present in 78.89% out of the 90 livers
dissected cases. 17,18
The aforementioned studies described the shape of sulcus (if
present) as scar, slit, and deep sulcus. The deep type of sulcus may
have a considerable length, breadth, and depth, and is divided into
open and closed type according to the medial end of it whether
open or closed. The scar type sulcus takes the shape of superficial
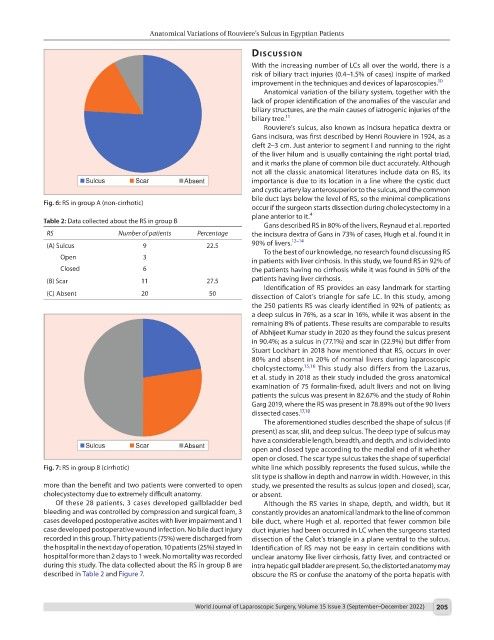
Fig. 7: RS in group B (cirrhotic) white line which possibly represents the fused sulcus, while the
slit type is shallow in depth and narrow in width. However, in this
more than the benefit and two patients were converted to open study, we presented the results as sulcus (open and closed), scar,
cholecystectomy due to extremely difficult anatomy. or absent.
Of these 28 patients, 3 cases developed gallbladder bed Although the RS varies in shape, depth, and width, but it
bleeding and was controlled by compression and surgical foam, 3 constantly provides an anatomical landmark to the line of common
cases developed postoperative ascites with liver impairment and 1 bile duct, where Hugh et al. reported that fewer common bile
case developed postoperative wound infection. No bile duct injury duct injuries had been occurred in LC when the surgeons started
recorded in this group. Thirty patients (75%) were discharged from dissection of the Calot’s triangle in a plane ventral to the sulcus.
the hospital in the next day of operation, 10 patients (25%) stayed in Identification of RS may not be easy in certain conditions with
hospital for more than 2 days to 1 week. No mortality was recorded unclear anatomy like liver cirrhosis, fatty liver, and contracted or
during this study. The data collected about the RS in group B are intra hepatic gall bladder are present. So, the distorted anatomy may
described in Table 2 and Figure 7. obscure the RS or confuse the anatomy of the porta hepatis with
World Journal of Laparoscopic Surgery, Volume 15 Issue 3 (September–December 2022) 205