Page 30 - tmp
P. 30
Laparoscopic Cholecystectomy
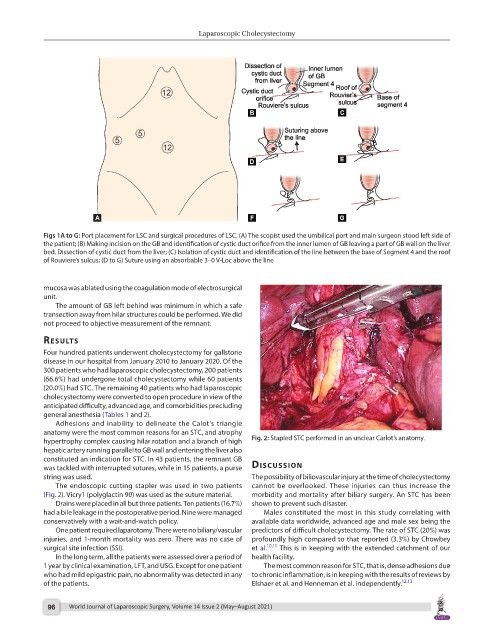
Figs 1A to G: Port placement for LSC and surgical procedures of LSC. (A) The scopist used the umbilical port and main surgeon stood left side of
the patient; (B) Making incision on the GB and identification of cystic duct orifice from the inner lumen of GB leaving a part of GB wall on the liver
bed. Dissection of cystic duct from the liver; (C) Isolation of cystic duct and identification of the line between the base of Segment 4 and the roof
of Rouviere’s sulcus; (D to G) Suture using an absorbable 3–0 V-Loc above the line
mucosa was ablated using the coagulation mode of electrosurgical
unit.
The amount of GB left behind was minimum in which a safe
transection away from hilar structures could be performed. We did
not proceed to objective measurement of the remnant.
results
Four hundred patients underwent cholecystectomy for gallstone
disease in our hospital from January 2010 to January 2020. Of the
300 patients who had laparoscopic cholecystectomy, 200 patients
(66.6%) had undergone total cholecystectomy while 60 patients
(20.0%) had STC. The remaining 40 patients who had laparoscopic
cholecystectomy were converted to open procedure in view of the
anticipated difficulty, advanced age, and comorbidities precluding
general anesthesia (Tables 1 and 2).
Adhesions and inability to delineate the Calot’s triangle
anatomy were the most common reasons for an STC, and atrophy
hypertrophy complex causing hilar rotation and a branch of high Fig. 2: Stapled STC performed in an unclear Carlot’s anatomy.
hepatic artery running parallel to GB wall and entering the liver also
constituted an indication for STC. In 43 patients, the remnant GB
was tackled with interrupted sutures, while in 15 patients, a purse dIscussIon
string was used. The possibility of biliovascular injury at the time of cholecystectomy
The endoscopic cutting stapler was used in two patients cannot be overlooked. These injuries can thus increase the
(Fig. 2). Vicry1 (polyglactin 90) was used as the suture material. morbidity and mortality after biliary surgery. An STC has been
Drains were placed in all but three patients. Ten patients (16.7%) shown to prevent such disaster.
had a bile leakage in the postoperative period. Nine were managed Males constituted the most in this study correlating with
conservatively with a wait-and-watch policy. available data worldwide, advanced age and male sex being the
One patient required laparotomy. There were no biliary/vascular predictors of difficult cholecystectomy. The rate of STC (20%) was
injuries, and 1-month mortality was zero. There was no case of profoundly high compared to that reported (3.3%) by Chowbey
surgical site infection (SSI). et al. 10,11 This is in keeping with the extended catchment of our
In the long term, all the patients were assessed over a period of health facility.
1 year by clinical examination, LFT, and USG. Except for one patient The most common reason for STC, that is, dense adhesions due
who had mild epigastric pain, no abnormality was detected in any to chronic inflammation, is in keeping with the results of reviews by
of the patients. Elshaer et al. and Henneman et al. independently. 12,13
96 World Journal of Laparoscopic Surgery, Volume 14 Issue 2 (May–August 2021)