Page 26 - tmp
P. 26
Laparoscopic Two-stage Hepatectomy
hepatic vein because insufficient FLR hypertrophy precluded right significance. Metastatic tumors tended to be fewer in the patients
hemihepatectomy. undergoing laparoscopic surgery. Although hepatectomy procedures
No morbidity or mortality followed the first-stage liver resection. differed between the laparoscopic and the open group at both first-
The second-stage resection was associated with no mortality, second-stage hepatectomy (p <0.001 and p = 0.013, respectively),
but two of three patients experienced operative morbidity. duration of the first-stage hepatectomy (p <0.01) and hospital stay
Complications after the second resection included a prolonged after the first-stage hepatectomy (p = 0.03) were shorter in patients
inflammatory state of unknown cause requiring antibiotic with laparoscopic resection than open resection. Total resected
administration (CD class I) in one patient and postoperative volume at second-stage hepatectomy was smaller in the laparoscopic
bleeding requiring surgical intervention (CD class IIIb) in another. group than in the open group (p = 0.016) because the procedures in
When these three patients were compared with 61 who the laparoscopic group had to be minimized because of insufficient
underwent an open first stage, small numbers precluded statistical remnant liver volume and functional hypertrophy (Table 2).
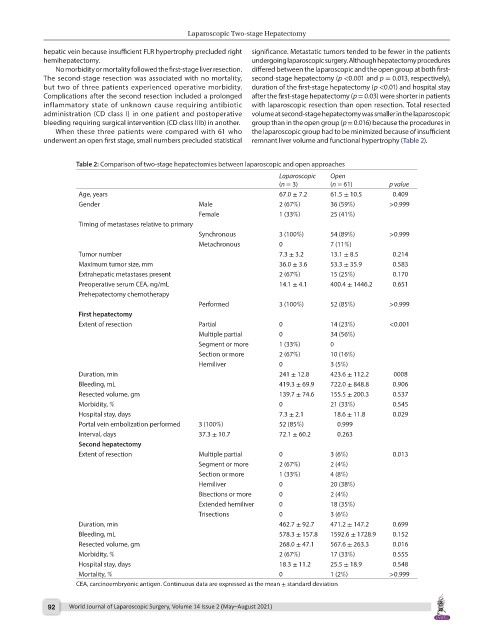
Table 2: Comparison of two-stage hepatectomies between laparoscopic and open approaches
Laparoscopic Open
(n = 3) (n = 61) p value
Age, years 67.0 ± 7.2 61.5 ± 10.5 0.409
Gender Male 2 (67%) 36 (59%) >0.999
Female 1 (33%) 25 (41%)
Timing of metastases relative to primary
Synchronous 3 (100%) 54 (89%) >0.999
Metachronous 0 7 (11%)
Tumor number 7.3 ± 3.2 13.1 ± 8.5 0.214
Maximum tumor size, mm 36.0 ± 3.6 53.3 ± 35.9 0.583
Extrahepatic metastases present 2 (67%) 15 (25%) 0.170
Preoperative serum CEA, ng/mL 14.1 ± 4.1 400.4 ± 1446.2 0.651
Prehepatectomy chemotherapy
Performed 3 (100%) 52 (85%) >0.999
First hepatectomy
Extent of resection Partial 0 14 (23%) <0.001
Multiple partial 0 34 (56%)
Segment or more 1 (33%) 0
Section or more 2 (67%) 10 (16%)
Hemiliver 0 3 (5%)
Duration, min 241 ± 12.8 423.6 ± 112.2 0008
Bleeding, mL 419.3 ± 69.9 722.0 ± 848.8 0.906
Resected volume, gm 139.7 ± 74.6 155.5 ± 200.3 0.537
Morbidity, % 0 21 (33%) 0.545
Hospital stay, days 7.3 ± 2.1 18.6 ± 11.8 0.029
Portal vein embolization performed 3 (100%) 52 (85%) 0.999
Interval, days 37.3 ± 10.7 72.1 ± 60.2 0.263
Second hepatectomy
Extent of resection Multiple partial 0 3 (6%) 0.013
Segment or more 2 (67%) 2 (4%)
Section or more 1 (33%) 4 (8%)
Hemiliver 0 20 (38%)
Bisections or more 0 2 (4%)
Extended hemiliver 0 18 (35%)
Trisections 0 3 (6%)
Duration, min 462.7 ± 92.7 471.2 ± 147.2 0.699
Bleeding, mL 578.3 ± 157.8 1592.6 ± 1728.9 0.152
Resected volume, gm 268.0 ± 47.1 567.6 ± 263.3 0.016
Morbidity, % 2 (67%) 17 (33%) 0.555
Hospital stay, days 18.3 ± 11.2 25.5 ± 18.9 0.548
Mortality, % 0 1 (2%) >0.999
CEA, carcinoembryonic antigen. Continuous data are expressed as the mean ± standard deviation
92 World Journal of Laparoscopic Surgery, Volume 14 Issue 2 (May–August 2021)