Page 33 - tmp
P. 33
Comparative Evaluation of Vaginoscopy vs Traditional Hysteroscopy
May 2019. The study included 100 women aged 20 to 60 years old and socioeconomic status between patients of groups A and
including nulliparous, multiparous, and postmenopausal. These 100 B were observed.
women were randomly allocated into two groups. Group A had 50 Data on pain score at various stages are shown in Table 2.
women who had undergone traditional hysteroscopy and group Analysis showed that the p value was 0.026, i.e., a significant
B had 50 women who had undergone vaginoscopic hysteroscopy. difference was found in the pain score. A maximum number of
Few patients were lost to follow-up. Eventually, 44 patients were patients (68%) perceived the pain of grade 4 during the grasping
included in group A and 42 patients in group B (Fig. 1). of the cervix with vulselum during the traditional hysteroscopy.
In vaginoscopic hysteroscopy as there is direct introduction of
Selection of Cases hysteroscope, pain is perceived only in two steps.
• All patients of infertility. No-touch vaginoscopic hysteroscopy was quicker to perform.
• Dysfunctional uterine bleeding (DUB). Time required in the procedures is summarized in Table 3. In the
• Postmenopausal bleeding. diagnostic study during vaginoscopic procedure, 32 patients
• Other gynecological complaints in which hysteroscopy (76.19%) had completed their procedure in between 3 and
indicated. 5 minutes. In traditional hysteroscopy, procedure time is 5 to
7 minutes in 34 patients (77.27%).
Exclusion Criteria No major side effects were recorded during the procedure
• Pregnant women. performed in any of the groups. The procedure failed in few
• Cancer of the cervix. patients, the most common cause being cervical stenosis.
• Active infection of the genital tract.
• Cardiovascular disease.
• Severe obstructive airway disease.
• Acute generalized peritonitis. Table 1: Comparative evaluation of demographic distribution of patients
• Blood dyscrasias and coagulopathy. Group B
Group A (Traditional) (Vaginoscopic)
A thorough history was taken which included menstrual history, N = 44 N = 42
obstetrical history, and medical history, including any history of Age (years)
diabetes, hypertension, and cardiovascular disease. Personal history <20 00 0 0 0
regarding smoking and alcohol intake was taken. 20–29 10 22.7% 08 42.8%
General examination and systemic examination were done. 30–39 17 38.6% 14 33%
Basic routine blood investigations were done. Transabdominal 40–49 09 20.4% 10 23.8%
ultrasound and transvaginal sonography were done where >50 08 18.1% 10 23.8%
indicated. Parity
A simple hysteroscope with a telescope of rigid 4 mm Nulliparous 7 15.9% 08 19%
diameter was used. The timing of the examination was during Multiparous 21 47.7% 24 57.1%
the proliferative phase of the menstrual cycle. The insertion Postmenopausal 16 36.3% 10 23.8%
of hysteroscope through cervical canal was done under direct Socioeconomic status
vision and in vaginoscopy without cervical dilatation or passage Low 25 56.8% 24 57.1%
of sound as a tight cervix acts as a good seal to prevent leakage Middle 14 31.8% 12 28.5%
of the distending media and allow examination of the cervical Upper 05 11.3% 06 14.2%
Habitat
canal and inspection of undamaged endometrium. Pain score Rural 24 54.5% 22 52.3%
(according to Wong–Baker Faces pain rating scale), procedure Urban 20 45.4% 20 47.6%
time, and complications were noted.
results Table 2: Evaluation of pain
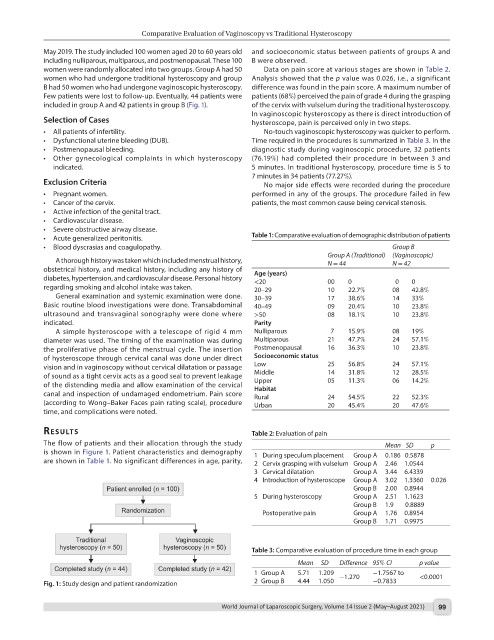
The flow of patients and their allocation through the study Mean SD p
is shown in Figure 1. Patient characteristics and demography 1 During speculum placement Group A 0.186 0.5878
are shown in Table 1. No significant differences in age, parity, 2 Cervix grasping with vulselum Group A 2.46 1.0544
3 Cervical dilatation Group A 3.44 6.4339
4 Introduction of hysteroscope Group A 3.02 1.3360 0.026
Group B 2.00 0.8944
5 During hysteroscopy Group A 2.51 1.1623
Group B 1.9 0.8889
Postoperative pain Group A 1.76 0.8954
Group B 1.71 0.9975
Table 3: Comparative evaluation of procedure time in each group
Mean SD Difference 95% CI p value
1 Group A 5.71 1.209 −1.270 −1.7567 to <0.0001
Fig. 1: Study design and patient randomization 2 Group B 4.44 1.050 −0.7833
World Journal of Laparoscopic Surgery, Volume 14 Issue 2 (May–August 2021) 99