Page 34 - tmp
P. 34
Comparative Evaluation of Vaginoscopy vs Traditional Hysteroscopy
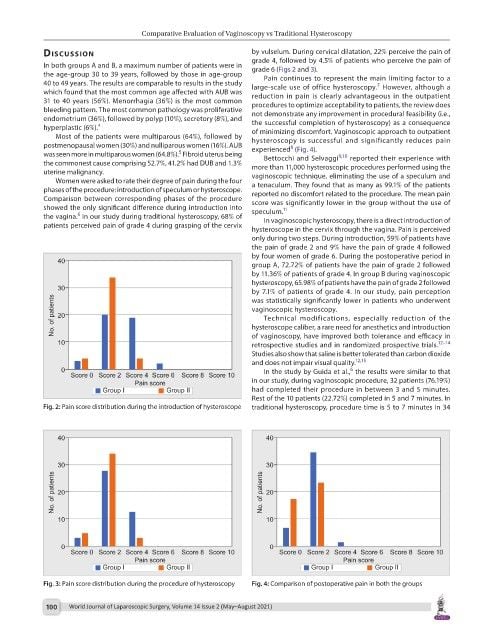
dIscussIon by vulselum. During cervical dilatation, 22% perceive the pain of
In both groups A and B, a maximum number of patients were in grade 4, followed by 4.5% of patients who perceive the pain of
grade 6 (Figs 2 and 3).
the age-group 30 to 39 years, followed by those in age-group Pain continues to represent the main limiting factor to a
40 to 49 years. The results are comparable to results in the study large-scale use of office hysteroscopy. However, although a
7
which found that the most common age affected with AUB was reduction in pain is clearly advantageous in the outpatient
31 to 40 years (56%). Menorrhagia (36%) is the most common procedures to optimize acceptability to patients, the review does
bleeding pattern. The most common pathology was proliferative not demonstrate any improvement in procedural feasibility (i.e.,
endometrium (36%), followed by polyp (10%), secretory (8%), and the successful completion of hysteroscopy) as a consequence
hyperplastic (6%). 4 of minimizing discomfort. Vaginoscopic approach to outpatient
Most of the patients were multiparous (64%), followed by hysteroscopy is successful and significantly reduces pain
postmenopausal women (30%) and nulliparous women (16%). AUB experienced (Fig. 4).
8
5
was seen more in multiparous women (64.8%). Fibroid uterus being Bettocchi and Selvaggi 9,10 reported their experience with
the commonest cause comprising 52.7%, 41.2% had DUB and 1.3% more than 11,000 hysteroscopic procedures performed using the
uterine malignancy. vaginoscopic technique, eliminating the use of a speculum and
Women were asked to rate their degree of pain during the four a tenaculum. They found that as many as 99.1% of the patients
phases of the procedure: introduction of speculum or hysteroscope. reported no discomfort related to the procedure. The mean pain
Comparison between corresponding phases of the procedure score was significantly lower in the group without the use of
showed the only significant difference during introduction into speculum. 11
6
the vagina. In our study during traditional hysteroscopy, 68% of In vaginoscopic hysteroscopy, there is a direct introduction of
patients perceived pain of grade 4 during grasping of the cervix
hysteroscope in the cervix through the vagina. Pain is perceived
only during two steps. During introduction, 59% of patients have
the pain of grade 2 and 9% have the pain of grade 4 followed
by four women of grade 6. During the postoperative period in
group A, 72.72% of patients have the pain of grade 2 followed
by 11.36% of patients of grade 4. In group B during vaginoscopic
hysteroscopy, 65.98% of patients have the pain of grade 2 followed
by 7.1% of patients of grade 4. In our study, pain perception
was statistically significantly lower in patients who underwent
vaginoscopic hysteroscopy.
Technical modifications, especially reduction of the
hysteroscope caliber, a rare need for anesthetics and introduction
of vaginoscopy, have improved both tolerance and efficacy in
retrospective studies and in randomized prospective trials. 12–14
Studies also show that saline is better tolerated than carbon dioxide
and does not impair visual quality. 12,15
6
In the study by Guida et al., the results were similar to that
in our study, during vaginoscopic procedure, 32 patients (76.19%)
had completed their procedure in between 3 and 5 minutes.
Rest of the 10 patients (22.72%) completed in 5 and 7 minutes. In
Fig. 2: Pain score distribution during the introduction of hysteroscope traditional hysteroscopy, procedure time is 5 to 7 minutes in 34
Fig. 3: Pain score distribution during the procedure of hysteroscopy Fig. 4: Comparison of postoperative pain in both the groups
100 World Journal of Laparoscopic Surgery, Volume 14 Issue 2 (May–August 2021)