Page 52 - World Journal of Laparoscopic Surgery
P. 52
Role of Intraoperative ICG in Laparoscopic MALS Release
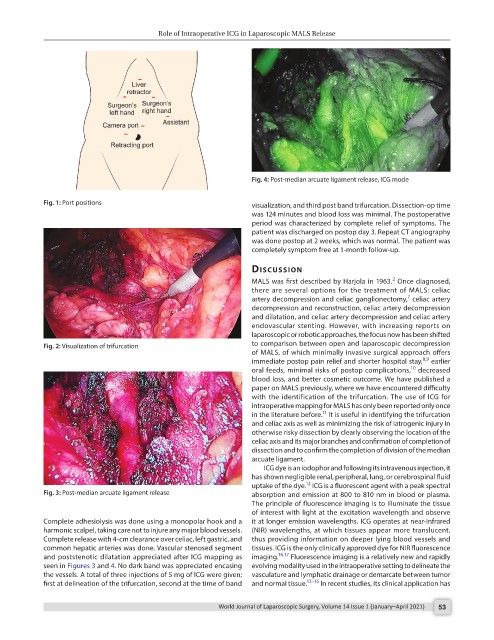
Fig. 4: Post-median arcuate ligament release, ICG mode
Fig. 1: Port positions visualization, and third post band trifurcation. Dissection-op time
was 124 minutes and blood loss was minimal. The postoperative
period was characterized by complete relief of symptoms. The
patient was discharged on postop day 3. Repeat CT angiography
was done postop at 2 weeks, which was normal. The patient was
completely symptom free at 1-month follow-up.
dIscussIon
2
MALS was first described by Harjola in 1963. Once diagnosed,
there are several options for the treatment of MALS: celiac
7
artery decompression and celiac ganglionectomy, celiac artery
decompression and reconstruction, celiac artery decompression
and dilatation, and celiac artery decompression and celiac artery
endovascular stenting. However, with increasing reports on
laparoscopic or robotic approaches, the focus now has been shifted
Fig. 2: Visualization of trifurcation to comparison between open and laparoscopic decompression
of MALS, of which minimally invasive surgical approach offers
8,9
immediate postop pain relief and shorter hospital stay, earlier
10
oral feeds, minimal risks of postop complications, decreased
blood loss, and better cosmetic outcome. We have published a
paper on MALS previously, where we have encountered difficulty
with the identification of the trifurcation. The use of ICG for
intraoperative mapping for MALS has only been reported only once
11
in the literature before. It is useful in identifying the trifurcation
and celiac axis as well as minimizing the risk of iatrogenic injury in
otherwise risky dissection by clearly observing the location of the
celiac axis and its major branches and confirmation of completion of
dissection and to confirm the completion of division of the median
arcuate ligament.
ICG dye is an iodophor and following its intravenous injection, it
has shown negligible renal, peripheral, lung, or cerebrospinal fluid
12
uptake of the dye. ICG is a fluorescent agent with a peak spectral
Fig. 3: Post-median arcuate ligament release absorption and emission at 800 to 810 nm in blood or plasma.
The principle of fluorescence imaging is to illuminate the tissue
of interest with light at the excitation wavelength and observe
Complete adhesiolysis was done using a monopolar hook and a it at longer emission wavelengths. ICG operates at near-infrared
harmonic scalpel, taking care not to injure any major blood vessels. (NIR) wavelengths, at which tissues appear more translucent,
Complete release with 4-cm clearance over celiac, left gastric, and thus providing information on deeper lying blood vessels and
common hepatic arteries was done. Vascular stenosed segment tissues. ICG is the only clinically approved dye for NIR fluorescence
and poststenotic dilatation appreciated after ICG mapping as imaging. 16,17 Fluorescence imaging is a relatively new and rapidly
seen in Figures 3 and 4. No dark band was appreciated encasing evolving modality used in the intraoperative setting to delineate the
the vessels. A total of three injections of 5 mg of ICG were given; vasculature and lymphatic drainage or demarcate between tumor
first at delineation of the trifurcation, second at the time of band and normal tissue. 13–15 In recent studies, its clinical application has
World Journal of Laparoscopic Surgery, Volume 14 Issue 1 (January–April 2021) 53