Page 22 - World Journal of Laparoscopic Surgery
P. 22
Safety and Feasibility of Sleeve Gastrectomy with Loop Duodenal Switch
similar in the common channel subgroups in our study indicating
that the common channel length can be increased from 2.5 to
≥3 m in LDS surgeries, without altering metabolic efficacy. The
PR and DI% 10.94% 9.09% 11.32% anastomosis is placed distally in the ileum in LDS surgeries, and
this probably correlates with a potent ileal brake mediated by an
enhanced secretion of Peptide YY and GLP1 which stimulate early
1 year follow-up Mean ± SD 5.08 ± 0.76 (4–8.9) p < 0.001 4.63 ± 0.6 (4–6.2) 5.18 ± 0.76 (4–8.9) p = 0.029 CR% 89.06% 90.91% 88.68% p = 0.829 p = 0.178 satiety. 3
The resolution of hypertension, hyperlipidemia, and obstructive
sleep apnea was significant in our patients. Surve et al. showed
hypertension resolution of 75% and hyperlipidemia resolution of
26
94% following the SADS procedure. While Shoar et al. showed
hypertension resolution of 96.3% and hyperlipidemia resolution
of 68.3% and obstructive sleep apnea resolution of 63.3% after
LDS surgeries. 27
Major intraoperative complications were <1% and postoperative
complications requiring surgical intervention were <2% in our
N 64 11 53 N 64 11 53
patients. Surve et al. showed the short-term and long-term
complication rates of 4.3 and 0%, respectively, and zero mortality
PR and DI%
26
rate.
18.18%
18.18%
18.18%
The presence of loop anastomosis in LDS surgeries reduces the
chances of anastomotic leak and internal herniation by minimizing
6 months follow-up Mean ± SD 5.47 ± 0.81 (3.9–10) p < 0.001 5.28 ± 0.59 (4.6–6.5) 5.5 ± 0.85 (3.9–10) p = 0.41 CR% 81.82% 81.82% 81.82% p = 1 p = 0.186 the number of anastomoses and mesenteric gaps. To facilitate
tension-free anastomosis and make it technically simple, we
modified LDS surgery by dividing RGA at its origin and creating
a window in the lesser sac. This modification allows bringing the
duodenum down toward the ileum for the anastomosis, rather
than taking ileum to the first part of the duodenum into the right
subhepatic space. This modification results in a freely mobile sleeve,
pylorus, and the first part of the duodenum, facilitating tension-
free anastomosis and avoids the need to divide greater omentum
N 77 11 66 N 77 11 66 to facilitate the same. None of our patents required division of
greater omentum. Sánchez-Pernaute et al. in their proposed SADI-S
CR, complete diabetes remission, PR and DI, partial diabetes remission and diabetes improvement
7
technique did not divide RGA. Dallegrave proposed division of RGA
8
while performing LDS surgeries. He suggested that the division
of RGA reduces the risk of marginal ulcers and bile reflux. A large
—
—
—
—
gap is left behind anastomosis in our modification. This large gap
Preoperative Mean ± SD 8.71 ± 1.82 (5–12.1) 8.91 ± 2.07 (6.1–11.8) 8.67 ± 1.79 (5–12.1) p = 0.694 perhaps allows free movement of intestinal loops behind without
causing an obstruction. None of our patients developed obstruction
or strangulation due to internal herniation. Gebelli et al. showed
9
that LDS surgeries with RGA ligation can be performed safely.
Preservation of the pylorus reduces the risk of acid exposure
—
—
—
—
to the anastomosis, thereby reducing the risk of marginal ulcers.
d Common channel length was taken as an independent variable
In their pooled analysis, Surve et al. showed that the anastomotic
leak, ulcer, and bile reflux occurred in 0.6% (9/1328), 0.1% (2/1328),
N 82 11 71 — — — — and 0.1% (2/1328), respectively. None of their patients had an
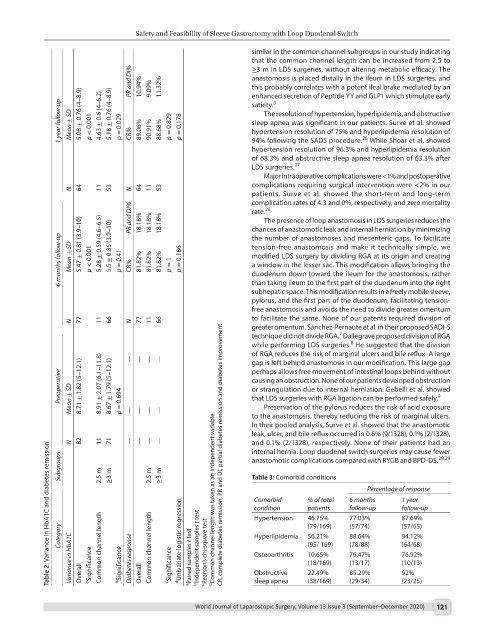
Table 2: Variance in HbA1C and diabetes remission
internal hernia. Loop duodenal switch surgeries may cause fewer
Subgroups 2.5 m ≥3 m 2.5 m ≥3 m anastomotic complications compared with RYGB and BPD-DS.
28,29
Table 3: Comorbid conditions
Percentage of response
1 year
% of total
6 months
Comorbid
follow-up
follow-up
condition
patients
(57/65)
(57/74)
(79/169)
Category d Univariate logistic regression Hypertension 46.75% 77.03% 87.69%
88.64%
94.12%
56.21%
Hyperlipidemia
Variance in HbA1C Overall a Significance Common channel length b Significance Diabetes response Overall Common channel length c Significance a Paired samples t test b Independent samples t test c Pearson’s chi-square test Osteoarthritis 10.65% 76.47% 76.92%
(95/ 169)
(64/68)
(78/88)
(13/17)
(18/169)
(10/13)
92%
Obstructive
22.49%
85.29%
(23/25)
sleep apnea
(29/34)
(38/169)
World Journal of Laparoscopic Surgery, Volume 13 Issue 3 (September–December 2020) 121