Page 5 - World Journal of Laparoscopic Surgery
P. 5
Complications of Laparoscopic Cholecystectomy
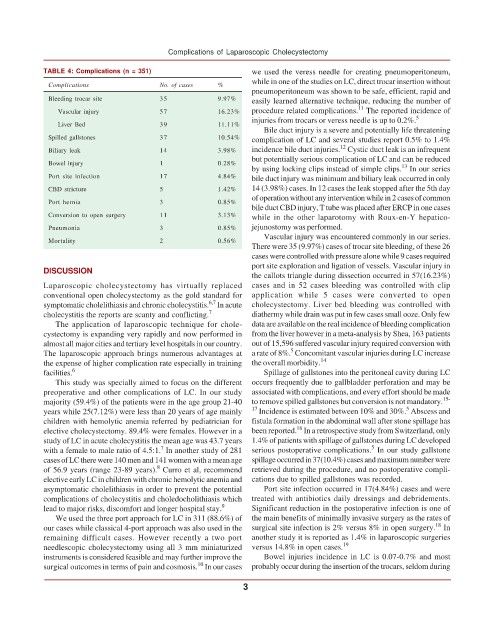
TABLE 4: Complications (n = 351) we used the veress needle for creating pneumoperitoneum,
while in one of the studies on LC, direct trocar insertion without
Complications No. of cases %
pneumoperitoneum was shown to be safe, efficient, rapid and
Bleeding trocar site 35 9.97% easily learned alternative technique, reducing the number of
11
Vascular injury 57 16.23% procedure related complications. The reported incidence of
injuries from trocars or veress needle is up to 0.2%. 5
Liver Bed 39 11.11%
Bile duct injury is a severe and potentially life threatening
Spilled gallstones 37 10.54% complication of LC and several studies report 0.5% to 1.4%
12
Biliary leak 14 3.98% incidence bile duct injuries. Cystic duct leak is an infrequent
but potentially serious complication of LC and can be reduced
Bowel injury 1 0.28%
13
by using locking clips instead of simple clips. In our series
Port site infection 17 4.84% bile duct injury was minimum and biliary leak occurred in only
CBD stricture 5 1.42% 14 (3.98%) cases. In 12 cases the leak stopped after the 5th day
of operation without any intervention while in 2 cases of common
Port hernia 3 0.85%
bile duct CBD injury, T tube was placed after ERCP in one cases
Conversion to open surgery 11 3.13% while in the other laparotomy with Roux-en-Y hepatico-
Pneumonia 3 0.85% jejunostomy was performed.
Vascular injury was encountered commonly in our series.
Mortality 2 0.56%
There were 35 (9.97%) cases of trocar site bleeding, of these 26
cases were controlled with pressure alone while 9 cases required
port site exploration and ligation of vessels. Vascular injury in
DISCUSSION
the callots triangle during dissection occurred in 57(16.23%)
Laparoscopic cholecystectomy has virtually replaced cases and in 52 cases bleeding was controlled with clip
conventional open cholecystectomy as the gold standard for application while 5 cases were converted to open
6,7
symptomatic cholelithiasis and chronic cholecystitis. In acute cholecystectomy. Liver bed bleeding was controlled with
cholecystitis the reports are scanty and conflicting. 7 diathermy while drain was put in few cases small ooze. Only few
The application of laparoscopic technique for chole- data are available on the real incidence of bleeding complication
cystectomy is expanding very rapidly and now performed in from the liver however in a meta-analysis by Shea, 163 patients
almost all major cities and tertiary level hospitals in our country. out of 15,596 suffered vascular injury required conversion with
5
The laparoscopic approach brings numerous advantages at a rate of 8%. Concomitant vascular injuries during LC increase
the expense of higher complication rate especially in training the overall morbidity. 14
facilities. 6 Spillage of gallstones into the peritoneal cavity during LC
This study was specially aimed to focus on the different occurs frequently due to gallbladder perforation and may be
preoperative and other complications of LC. In our study associated with complications, and every effort should be made
majority (59.4%) of the patients were in the age group 21-40 to remove spilled gallstones but conversion is not mandatory. 15-
5
years while 25(7.12%) were less than 20 years of age mainly 17 Incidence is estimated between 10% and 30%. Abscess and
children with hemolytic anemia referred by pediatrician for fistula formation in the abdominal wall after stone spillage has
16
elective cholecystectomy. 89.4% were females. However in a been reported. In a retrospective study from Switzerland, only
study of LC in acute cholecystitis the mean age was 43.7 years 1.4% of patients with spillage of gallstones during LC developed
5
7
with a female to male ratio of 4.5:1. In another study of 281 serious postoperative complications. In our study gallstone
cases of LC there were 140 men and 141 women with a mean age spillage occurred in 37(10.4%) cases and maximum number were
8
of 56.9 years (range 23-89 years). Curro et al, recommend retrieved during the procedure, and no postoperative compli-
elective early LC in children with chronic hemolytic anemia and cations due to spilled gallstones was recorded.
asymptomatic cholelithiasis in order to prevent the potential Port site infection occurred in 17(4.84%) cases and were
complications of cholecystitis and choledocholithiasis which treated with antibiotics daily dressings and debridements.
lead to major risks, discomfort and longer hospital stay. 9 Significant reduction in the postoperative infection is one of
We used the three port approach for LC in 311 (88.6%) of the main benefits of minimally invasive surgery as the rates of
18
our cases while classical 4-port approach was also used in the surgical site infection is 2% versus 8% in open surgery. In
remaining difficult cases. However recently a two port another study it is reported as 1.4% in laparoscopic surgeries
needlescopic cholecystectomy using all 3 mm miniaturized versus 14.8% in open cases. 19
instruments is considered feasible and may further improve the Bowel injuries incidence in LC is 0.07-0.7% and most
10
surgical outcomes in terms of pain and cosmosis. In our cases probably occur during the insertion of the trocars, seldom during
3