Page 4 - World Journal of Laparoscopic Surgery
P. 4
Rooh-ul-Muqim et al
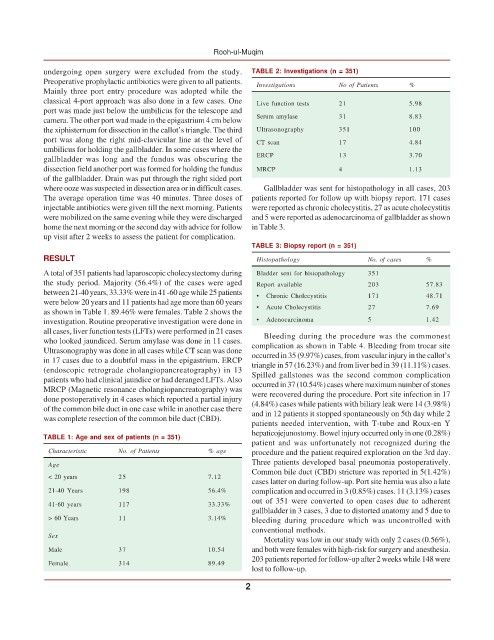
undergoing open surgery were excluded from the study. TABLE 2: Investigations (n = 351)
Preoperative prophylactic antibiotics were given to all patients. Investigations No of Patients %
Mainly three port entry procedure was adopted while the
classical 4-port approach was also done in a few cases. One Live function tests 21 5.98
port was made just below the umbilicus for the telescope and
camera. The other port wad made in the epigastrium 4 cm below Serum amylase 31 8.83
the xiphisternum for dissection in the callot’s triangle. The third Ultrasonography 351 100
port was along the right mid-clavicular line at the level of CT scan 17 4.84
umbilicus for holding the gallbladder. In some cases where the
gallbladder was long and the fundus was obscuring the ERCP 13 3.70
dissection field another port was formed for holding the fundus MRCP 4 1.13
of the gallbladder. Drain was put through the right sided port
where ooze was suspected in dissection area or in difficult cases. Gallbladder was sent for histopathology in all cases, 203
The average operation time was 40 minutes. Three doses of patients reported for follow up with biopsy report. 171 cases
injectable antibiotics were given till the next morning. Patients were reported as chronic cholecystitis, 27 as acute cholecystitis
were mobilized on the same evening while they were discharged and 5 were reported as adenocarcinoma of gallbladder as shown
home the next morning or the second day with advice for follow in Table 3.
up visit after 2 weeks to assess the patient for complication.
TABLE 3: Biopsy report (n = 351)
RESULT Histopathology No. of cases %
A total of 351 patients had laparoscopic cholecystectomy during Bladder sent for histopathology 351
the study period. Majority (56.4%) of the cases were aged Report available 203 57.83
between 21-40 years, 33.33% were in 41 -60 age while 25 patients • Chronic Cholecystitis 171 48.71
were below 20 years and 11 patients had age more than 60 years
as shown in Table 1. 89.46% were females. Table 2 shows the • Acute Cholecystitis 27 7.69
investigation. Routine preoperative investigation were done in • Adenocarcinoma 5 1.42
all cases, liver function tests (LFTs) were performed in 21 cases Bleeding during the procedure was the commonest
who looked jaundiced. Serum amylase was done in 11 cases. complication as shown in Table 4. Bleeding from trocar site
Ultrasonography was done in all cases while CT scan was done occurred in 35 (9.97%) cases, from vascular injury in the callot’s
in 17 cases due to a doubtful mass in the epigastrium. ERCP triangle in 57 (16.23%) and from liver bed in 39 (11.11%) cases.
(endoscopic retrograde cholangiopancreatography) in 13 Spilled gallstones was the second common complication
patients who had clinical jaundice or had deranged LFTs. Also occurred in 37 (10.54%) cases where maximum number of stones
MRCP (Magnetic resonance cholangiopancreatography) was were recovered during the procedure. Port site infection in 17
done postoperatively in 4 cases which reported a partial injury (4.84%) cases while patients with biliary leak were 14 (3.98%)
of the common bile duct in one case while in another case there and in 12 patients it stopped spontaneously on 5th day while 2
was complete resection of the common bile duct (CBD).
patients needed intervention, with T-tube and Roux-en Y
hepaticojejunostomy. Bowel injury occurred only in one (0.28%)
TABLE 1: Age and sex of patients (n = 351)
patient and was unfortunately not recognized during the
Characteristic No. of Patients % age procedure and the patient required exploration on the 3rd day.
Three patients developed basal pneumonia postoperatively.
Age
Common bile duct (CBD) stricture was reported in 5(1.42%)
< 20 years 25 7.12
cases latter on during follow-up. Port site hernia was also a late
21-40 Years 198 56.4% complication and occurred in 3 (0.85%) cases. 11 (3.13%) cases
out of 351 were converted to open cases due to adherent
41-60 years 117 33.33%
gallbladder in 3 cases, 3 due to distorted anatomy and 5 due to
> 60 Years 11 3.14% bleeding during procedure which was uncontrolled with
conventional methods.
Sex
Mortality was low in our study with only 2 cases (0.56%),
Male 37 10.54 and both were females with high-risk for surgery and anesthesia.
203 patients reported for follow-up after 2 weeks while 148 were
Female 314 89.49
lost to follow-up.
2