Page 35 - World Journal of Laparoscopic Surgery
P. 35
Comparison of Drugs and Intravenous Crystalloid in Reduction of Postoperative Nausea and Vomiting after Lap Surgery
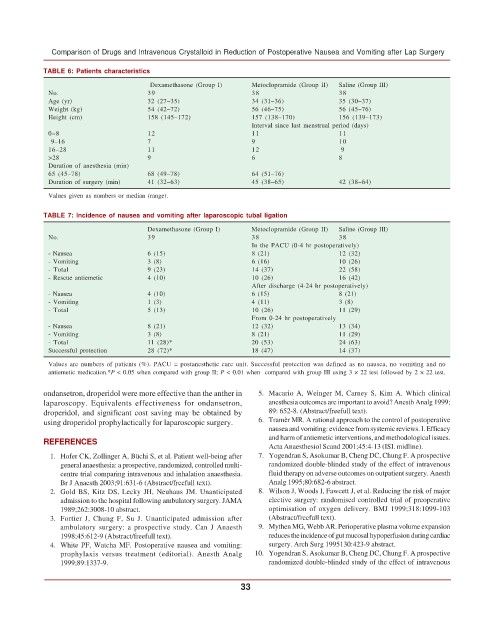
TABLE 6: Patients characteristics
Dexamethasone (Group I) Metoclopramide (Group II) Saline (Group III)
No. 39 38 38
Age (yr) 32 (27–35) 34 (31–36) 35 (30–37)
Weight (kg) 54 (42–72) 56 (46–75) 56 (45–76)
Height (cm) 158 (145–172) 157 (138–170) 156 (139–173)
Interval since last menstrual period (days)
0–8 12 11 11
9–16 7 9 10
16–28 11 12 9
>28 9 6 8
Duration of anesthesia (min)
65 (45–78) 68 (49–78) 64 (51–76)
Duration of surgery (min) 41 (32–63) 45 (38–65) 42 (38–64)
Values given as numbers or median (range).
TABLE 7: Incidence of nausea and vomiting after laparoscopic tubal ligation
Dexamethasone (Group I) Metoclopramide (Group II) Saline (Group III)
No. 39 38 38
In the PACU (0-4 hr postoperatively)
- Nausea 6 (15) 8 (21) 12 (32)
- Vomiting 3 (8) 6 (16) 10 (26)
- Total 9 (23) 14 (37) 22 (58)
- Rescue antiemetic 4 (10) 10 (26) 16 (42)
After discharge (4-24 hr postoperatively)
- Nausea 4 (10) 6 (15) 8 (21)
- Vomiting 1 (3) 4 (11) 3 (8)
- Total 5 (13) 10 (26) 11 (29)
From 0-24 hr postoperatively
- Nausea 8 (21) 12 (32) 13 (34)
- Vomiting 3 (8) 8 (21) 11 (29)
- Total 11 (28)* 20 (53) 24 (63)
Successful protection 28 (72)* 18 (47) 14 (37)
Values are numbers of patients (%). PACU = postanesthetic care unit. Successful protection was defined as no nausea, no vomiting and no
antiemetic medication.*P < 0.05 when compared with group II; P < 0.01 when compared with group III using 3 × 22 test followed by 2 × 22 test.
ondansetron, droperidol were more effective than the anther in 5. Macario A, Weinger M, Carney S, Kim A. Which clinical
laparoscopy. Equivalents effectiveness for ondansetron, anesthesia outcomes are important to avoid? Anesth Analg 1999;
droperidol, and significant cost saving may be obtained by 89: 652-8. (Abstract/freefull text).
using droperidol prophylactically for laparoscopic surgery. 6. Tramèr MR. A rational approach to the control of postoperative
nausea and vomiting: evidence from systemic reviews. I. Efficacy
and harm of antiemetic interventions, and methodological issues.
REFERENCES
Acta Anaesthesiol Scand 2001;45:4-13 (ISI. midline).
1. Hofer CK, Zollinger A, Büchi S, et al. Patient well-being after 7. Yogendran S, Asokumar B, Cheng DC, Chung F. A prospective
general anaesthesia: a prospective, randomized, controlled multi- randomized double-blinded study of the effect of intravenous
centre trial comparing intravenous and inhalation anaesthesia. fluid therapy on adverse outcomes on outpatient surgery. Anesth
Br J Anaesth 2003;91:631-6 (Abstract/freefull text). Analg 1995;80:682-6 abstract.
2. Gold BS, Kitz DS, Lecky JH, Neuhaus JM. Unanticipated 8. Wilson J, Woods I, Fawcett J, et al. Reducing the risk of major
admission to the hospital following ambulatory surgery. JAMA elective surgery: randomised controlled trial of preoperative
1989;262:3008-10 abstract. optimisation of oxygen delivery. BMJ 1999;318:1099-103
3. Fortier J, Chung F, Su J. Unanticipated admission after (Abstract/freefull text).
ambulatory surgery: a prospective study. Can J Anaesth 9. Mythen MG, Webb AR. Perioperative plasma volume expansion
1998;45:612-9 (Abstract/freefull text). reduces the incidence of gut mucosal hypoperfusion during cardiac
4. White PF, Watcha MF. Postoperative nausea and vomiting: surgery. Arch Surg 1995130:423-9 abstract.
prophylaxis versus treatment (editorial). Anesth Analg 10. Yogendran S, Asokumar B, Cheng DC, Chung F. A prospective
1999;89:1337-9. randomized double-blinded study of the effect of intravenous
33