Page 33 - World Journal of Laparoscopic Surgery
P. 33
Comparison of Drugs and Intravenous Crystalloid in Reduction of Postoperative Nausea and Vomiting after Lap Surgery
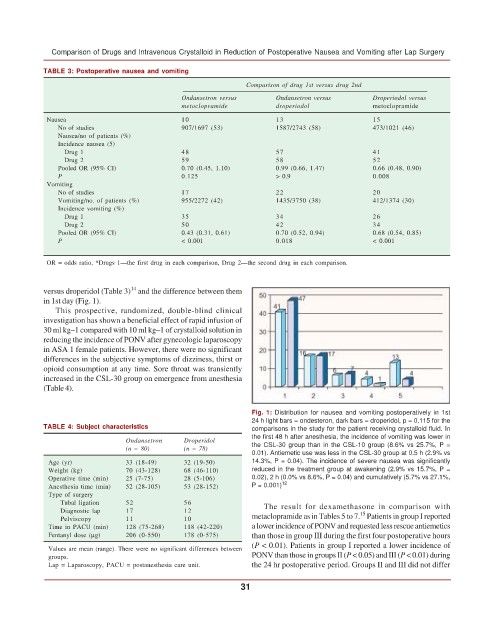
TABLE 3: Postoperative nausea and vomiting
Comparison of drug 1st versus drug 2nd
Ondansetron versus Ondansetron versus Droperiodol versus
metoclopramide droperiodol metoclopramide
Nausea 10 13 15
No of studies 907/1697 (53) 1587/2743 (58) 473/1021 (46)
Nausea/no of patients (%)
Incidence nausea (5)
Drug 1 48 57 41
Drug 2 59 58 52
Pooled OR (95% CI) 0.70 (0.45, 1.10) 0.99 (0.66, 1.47) 0.66 (0.48, 0.90)
P 0.125 > 0.9 0.008
Vomiting
No of studies 17 22 20
Vomiting/no. of patients (%) 955/2272 (42) 1435/3750 (38) 412/1374 (30)
Incidence vomiting (%)
Drug 1 35 34 26
Drug 2 50 42 34
Pooled OR (95% CI) 0.43 (0.31, 0.61) 0.70 (0.52, 0.94) 0.68 (0.54, 0.85)
P < 0.001 0.018 < 0.001
OR = odds ratio, *Drugs 1—the first drug in each comparison, Drug 2—the second drug in each comparison.
14
versus droperidol (Table 3) and the difference between them
in 1st day (Fig. 1).
This prospective, randomized, double-blind clinical
investigation has shown a beneficial effect of rapid infusion of
30 ml kg–1 compared with 10 ml kg–1 of crystalloid solution in
reducing the incidence of PONV after gynecologic laparoscopy
in ASA 1 female patients. However, there were no significant
differences in the subjective symptoms of dizziness, thirst or
opioid consumption at any time. Sore throat was transiently
increased in the CSL-30 group on emergence from anesthesia
(Table 4).
Fig. 1: Distribution for nausea and vomiting postoperatively in 1st
24 h light bars = ondesteron, dark bars = droperidol, p = 0.115 for the
TABLE 4: Subject characteristics comparisons in the study for the patient receiving crystalloid fluid. In
the first 48 h after anesthesia, the incidence of vomiting was lower in
Ondansetron Droperidol the CSL-30 group than in the CSL-10 group (8.6% vs 25.7%, P =
(n = 80) (n = 78)
0.01). Antiemetic use was less in the CSL-30 group at 0.5 h (2.9% vs
Age (yr) 33 (18-49) 32 (19-50) 14.3%, P = 0.04). The incidence of severe nausea was significantly
Weight (kg) 70 (43-128) 68 (46-110) reduced in the treatment group at awakening (2.9% vs 15.7%, P =
Operative time (min) 25 (7-75) 28 (5-106) 0.02), 2 h (0.0% vs 8.6%, P = 0.04) and cumulatively (5.7% vs 27.1%,
Anesthesia time (min) 52 (28-105) 53 (28-152) P = 0.001) 12
Type of surgery
Tubal ligation 52 56 The result for dexamethasone in comparison with
Diagnostic lap 17 12 metaclopramide as in Tables 5 to 7. Patients in group I reported
15
Pelviscopy 11 10
Time in PACU (min) 128 (75-268) 118 (42-220) a lower incidence of PONV and requested less rescue antiemetics
Fentanyl dose (μg) 206 (0-550) 178 (0-575) than those in group III during the first four postoperative hours
(P < 0.01). Patients in group I reported a lower incidence of
Values are mean (range). There were no significant differences between
groups. PONV than those in groups II (P < 0.05) and III (P < 0.01) during
Lap = Laparoscopy, PACU = postanesthesia care unit. the 24 hr postoperative period. Groups II and III did not differ
31