Page 18 - World Journal of Laparoscopic Surgery
P. 18
Laparoscopic Cholecystectomy in Patients Over 80 Years is Feasible and Safe: Analysis of 68 Consecutive Cases
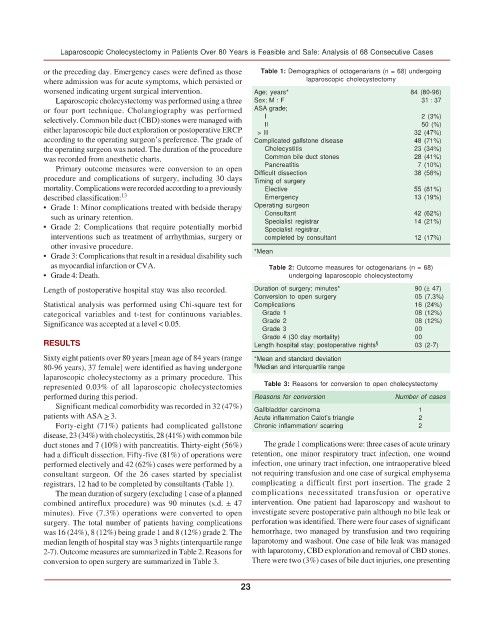
or the preceding day. Emergency cases were defined as those Table 1: Demographics of octogenarians (n = 68) undergoing
where admission was for acute symptoms, which persisted or laparoscopic cholecystectomy
worsened indicating urgent surgical intervention. Age; years* 84 (80-96)
Laparoscopic cholecystectomy was performed using a three Sex; M : F 31 : 37
or four port technique. Cholangiography was performed ASA grade;
selectively. Common bile duct (CBD) stones were managed with I II 2 (3%)
50 (%)
either laparoscopic bile duct exploration or postoperative ERCP > III 32 (47%)
according to the operating surgeon’s preference. The grade of Complicated gallstone disease 48 (71%)
the operating surgeon was noted. The duration of the procedure Cholecystitis 23 (34%)
was recorded from anesthetic charts. Common bile duct stones 28 (41%)
Primary outcome measures were conversion to an open Pancreatitis 7 (10%)
procedure and complications of surgery, including 30 days Difficult dissection 38 (56%)
Timing of surgery
mortality. Complications were recorded according to a previously Elective 55 (81%)
described classification: 13 Emergency 13 (19%)
• Grade 1: Minor complications treated with bedside therapy Operating surgeon
such as urinary retention. Consultant 42 (62%)
• Grade 2: Complications that require potentially morbid Specialist registrar 14 (21%)
Specialist registrar,
interventions such as treatment of arrhythmias, surgery or completed by consultant 12 (17%)
other invasive procedure.
• Grade 3: Complications that result in a residual disability such *Mean
as myocardial infarction or CVA. Table 2: Outcome measures for octogenarians (n = 68)
• Grade 4: Death. undergoing laparoscopic cholecystectomy
Length of postoperative hospital stay was also recorded. Duration of surgery; minutes* 90 (± 47)
Conversion to open surgery 05 (7.3%)
Statistical analysis was performed using Chi-square test for Complications 16 (24%)
categorical variables and t-test for continuous variables. Grade 1 08 (12%)
Significance was accepted at a level < 0.05. Grade 2 08 (12%)
Grade 3 00
Grade 4 (30 day mortality) 00
RESULTS Length hospital stay; postoperative nights § 03 (2-7)
Sixty eight patients over 80 years [mean age of 84 years (range *Mean and standard deviation
80-96 years), 37 female] were identified as having undergone § Median and interquartile range
laparoscopic cholecystectomy as a primary procedure. This
represented 0.03% of all laparoscopic cholecystectomies Table 3: Reasons for conversion to open cholecystectomy
performed during this period. Reasons for conversion Number of cases
Significant medical comorbidity was recorded in 32 (47%) Gallbladder carcinoma 1
patients with ASA > 3. Acute inflammation Calot’s triangle 2
Forty-eight (71%) patients had complicated gallstone Chronic inflammation/ scarring 2
disease, 23 (34%) with cholecystitis, 28 (41%) with common bile
duct stones and 7 (10%) with pancreatitis. Thirty-eight (56%) The grade 1 complications were: three cases of acute urinary
had a difficult dissection. Fifty-five (81%) of operations were retention, one minor respiratory tract infection, one wound
performed electively and 42 (62%) cases were performed by a infection, one urinary tract infection, one intraoperative bleed
consultant surgeon. Of the 26 cases started by specialist not requiring transfusion and one case of surgical emphysema
registrars, 12 had to be completed by consultants (Table 1). complicating a difficult first port insertion. The grade 2
The mean duration of surgery (excluding 1 case of a planned complications necessitated transfusion or operative
combined antireflux procedure) was 90 minutes (s.d. ± 47 intervention. One patient had laparoscopy and washout to
minutes). Five (7.3%) operations were converted to open investigate severe postoperative pain although no bile leak or
surgery. The total number of patients having complications perforation was identified. There were four cases of significant
was 16 (24%), 8 (12%) being grade 1 and 8 (12%) grade 2. The hemorrhage, two managed by transfusion and two requiring
median length of hospital stay was 3 nights (interquartile range laparotomy and washout. One case of bile leak was managed
2-7). Outcome measures are summarized in Table 2. Reasons for with laparotomy, CBD exploration and removal of CBD stones.
conversion to open surgery are summarized in Table 3. There were two (3%) cases of bile duct injuries, one presenting
23