Page 11 - World Journal of Laparoscopic Surgery
P. 11
Laparoscopic Dismembered Pyeloplasty: Our Experience in 15 Cases
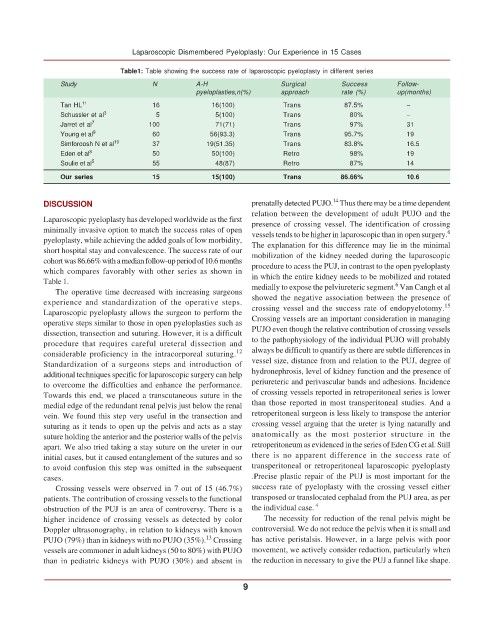
Table1: Table showing the success rate of laparoscopic pyeloplasty in different series
Study N A-H Surgical Success Follow-
pyeloplasties,n(%) approach rate (%) up(months)
Tan HL 11 16 16(100) Trans 87.5% –
Schussler et al 3 5 5(100) Trans 80% –
Jarret et al 7 100 71(71) Trans 97% 31
Young et al 9 60 56(93.3) Trans 95.7% 19
Simforoosh N et al 10 37 19(51.35) Trans 83.8% 16.5
Eden et al 8 50 50(100) Retro 98% 19
Soulie et al 5 55 48(87) Retro 87% 14
Our series 15 15(100) Trans 86.66% 10.6
14
DISCUSSION prenatally detected PUJO. Thus there may be a time dependent
relation between the development of adult PUJO and the
Laparoscopic pyeloplasty has developed worldwide as the first presence of crossing vessel. The identification of crossing
minimally invasive option to match the success rates of open vessels tends to be higher in laparoscopic than in open surgery. 6
pyeloplasty, while achieving the added goals of low morbidity,
short hospital stay and convalescence. The success rate of our The explanation for this difference may lie in the minimal
cohort was 86.66% with a median follow-up period of 10.6 months mobilization of the kidney needed during the laparoscopic
which compares favorably with other series as shown in procedure to acess the PUJ, in contrast to the open pyeloplasty
Table 1. in which the entire kidney needs to be mobilized and rotated
6
The operative time decreased with increasing surgeons medially to expose the pelviureteric segment. Van Cangh et al
experience and standardization of the operative steps. showed the negative association between the presence of
15
Laparoscopic pyeloplasty allows the surgeon to perform the crossing vessel and the success rate of endopyelotomy.
operative steps similar to those in open pyeloplasties such as Crossing vessels are an important consideration in managing
dissection, transection and suturing. However, it is a difficult PUJO even though the relative contribution of crossing vessels
procedure that requires careful ureteral dissection and to the pathophysiology of the individual PUJO will probably
considerable proficiency in the intracorporeal suturing. 12 always be difficult to quantify as there are subtle differences in
Standardization of a surgeons steps and introduction of vessel size, distance from and relation to the PUJ, degree of
additional techniques specific for laparoscopic surgery can help hydronephrosis, level of kidney function and the presence of
to overcome the difficulties and enhance the performance. periureteric and perivascular bands and adhesions. Incidence
Towards this end, we placed a transcutaneous suture in the of crossing vessels reported in retroperitoneal series is lower
medial edge of the redundant renal pelvis just below the renal than those reported in most transperitoneal studies. And a
vein. We found this step very useful in the transection and retroperitoneal surgeon is less likely to transpose the anterior
suturing as it tends to open up the pelvis and acts as a stay crossing vessel arguing that the ureter is lying naturally and
suture holding the anterior and the posterior walls of the pelvis anatomically as the most posterior structure in the
apart. We also tried taking a stay suture on the ureter in our retroperitoneum as evidenced in the series of Eden CG et al. Still
initial cases, but it caused entanglement of the sutures and so there is no apparent difference in the success rate of
to avoid confusion this step was omitted in the subsequent transperitoneal or retroperitoneal laparoscopic pyeloplasty
cases. .Precise plastic repair of the PUJ is most important for the
Crossing vessels were observed in 7 out of 15 (46.7%) success rate of pyeloplasty with the crossing vessel either
patients. The contribution of crossing vessels to the functional transposed or translocated cephalad from the PUJ area, as per
obstruction of the PUJ is an area of controversy. There is a the individual case. 4
higher incidence of crossing vessels as detected by color The necessity for reduction of the renal pelvis might be
Doppler ultrasonography, in relation to kidneys with known controversial. We do not reduce the pelvis when it is small and
13
PUJO (79%) than in kidneys with no PUJO (35%). Crossing has active peristalsis. However, in a large pelvis with poor
vessels are commoner in adult kidneys (50 to 80%) with PUJO movement, we actively consider reduction, particularly when
than in pediatric kidneys with PUJO (30%) and absent in the reduction in necessary to give the PUJ a funnel like shape.
9