Page 49 - World Journal of Laparoscopic Surgery
P. 49
Laparoscopic Instruments Marking Improve Length Measurement Precision
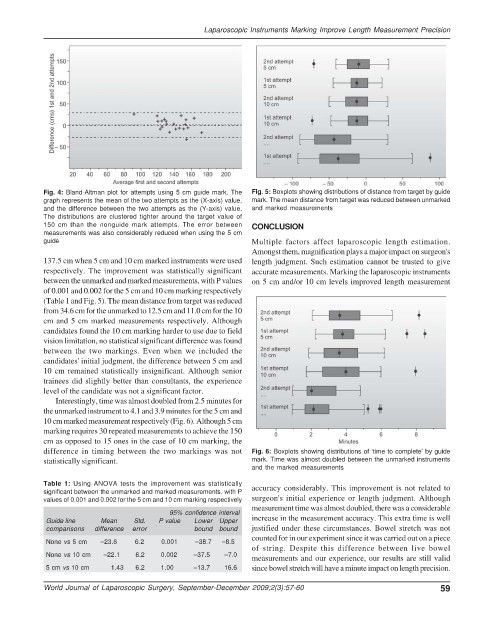
Fig. 4: Bland-Altman plot for attempts using 5 cm guide mark. The Fig. 5: Boxplots showing distributions of distance from target by guide
graph represents the mean of the two attempts as the (X-axis) value, mark. The mean distance from target was reduced between unmarked
and the difference between the two attempts as the (Y-axis) value. and marked measurements
The distributions are clustered tighter around the target value of
150 cm than the nonguide mark attempts. The error between CONCLUSION
measurements was also considerably reduced when using the 5 cm
guide Multiple factors affect laparoscopic length estimation.
Amongst them, magnification plays a major impact on surgeon's
137.5 cm when 5 cm and 10 cm marked instruments were used length judgment. Such estimation cannot be trusted to give
respectively. The improvement was statistically significant accurate measurements. Marking the laparoscopic instruments
between the unmarked and marked measurements, with P values on 5 cm and/or 10 cm levels improved length measurement
of 0.001 and 0.002 for the 5 cm and 10 cm marking respectively
(Table 1 and Fig. 5). The mean distance from target was reduced
from 34.6 cm for the unmarked to 12.5 cm and 11.0 cm for the 10
cm and 5 cm marked measurements respectively. Although
candidates found the 10 cm marking harder to use due to field
vision limitation, no statistical significant difference was found
between the two markings. Even when we included the
candidates' initial judgment, the difference between 5 cm and
10 cm remained statistically insignificant. Although senior
trainees did slightly better than consultants, the experience
level of the candidate was not a significant factor.
Interestingly, time was almost doubled from 2.5 minutes for
the unmarked instrument to 4.1 and 3.9 minutes for the 5 cm and
10 cm marked measurement respectively (Fig. 6). Although 5 cm
marking requires 30 repeated measurements to achieve the 150
cm as opposed to 15 ones in the case of 10 cm marking, the
difference in timing between the two markings was not Fig. 6: Boxplots showing distributions of ‘time to complete’ by guide
statistically significant. mark. Time was almost doubled between the unmarked instruments
and the marked measurements
Table 1: Using ANOVA tests the improvement was statistically accuracy considerably. This improvement is not related to
significant between the unmarked and marked measurements, with P
values of 0.001 and 0.002 for the 5 cm and 10 cm marking respectively surgeon's initial experience or length judgment. Although
measurement time was almost doubled, there was a considerable
95% confidence interval
Guide line Mean Std. P value Lower Upper increase in the measurement accuracy. This extra time is well
comparisons difference error bound bound justified under these circumstances. Bowel stretch was not
counted for in our experiment since it was carried out on a piece
None vs 5 cm –23.6 6.2 0.001 –38.7 –8.5
of string. Despite this difference between live bowel
None vs 10 cm –22.1 6.2 0.002 –37.5 –7.0
measurements and our experience, our results are still valid
5 cm vs 10 cm 1.43 6.2 1.00 –13.7 16.6 since bowel stretch will have a minute impact on length precision.
World Journal of Laparoscopic Surgery, September-December 2009;2(3):57-60 59