Page 27 - World Journal of Laparoscopic Surgery
P. 27
SB Naval
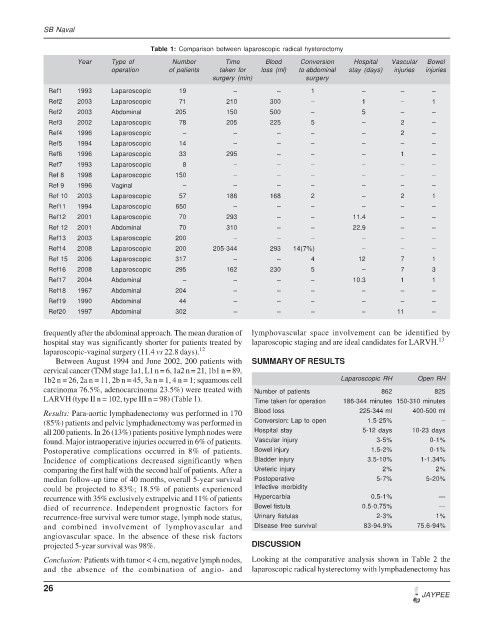
Table 1: Comparison between laparoscopic radical hysterectomy
Year Type of Number Time Blood Conversion Hospital Vascular Bowel
operation of patients taken for loss (ml) to abdominal stay (days) injuries injuries
surgery (min) surgery
Ref1 1993 Laparoscopic 19 – – 1 – – –
Ref2 2003 Laparoscopic 71 210 300 – 1 – 1
Ref2 2003 Abdominal 205 150 500 – 5 – –
Ref3 2002 Laparoscopic 78 205 225 5 – 2 –
Ref4 1996 Laparoscopic – – – – – 2 –
Ref5 1994 Laparoscopic 14 – – – – – –
Ref6 1996 Laparoscopic 33 295 – – – 1 –
Ref7 1993 Laparoscopic 8 – – – – – –
Ref 8 1998 Laparoscopic 150 – – – – – –
Ref 9 1996 Vaginal – – – – – – –
Ref 10 2003 Laparoscopic 57 186 168 2 – 2 1
Ref11 1994 Laparoscopic 650 – – – – – –
Ref12 2001 Laparoscopic 70 293 – – 11.4 – –
Ref 12 2001 Abdominal 70 310 – – 22.9 – –
Ref13 2003 Laparoscopic 200 – – – – – –
Ref14 2008 Laparoscopic 200 205-344 293 14(7%) – – –
Ref 15 2006 Laparoscopic 317 – – 4 12 7 1
Ref16 2008 Laparoscopic 295 162 230 5 – 7 3
Ref17 2004 Abdominal – – – – 10.3 1 1
Ref18 1967 Abdominal 204 – – – – – –
Ref19 1990 Abdominal 44 – – – – – –
Ref20 1997 Abdominal 302 – – – – 11 –
frequently after the abdominal approach. The mean duration of lymphovascular space involvement can be identified by
hospital stay was significantly shorter for patients treated by laparoscopic staging and are ideal candidates for LARVH. 13
laparoscopic-vaginal surgery (11.4 vs 22.8 days). 12
Between August 1994 and June 2002, 200 patients with SUMMARY OF RESULTS
cervical cancer (TNM stage 1a1, L1 n = 6, 1a2 n = 21, 1b1 n = 89,
1b2 n = 26, 2a n = 11, 2b n = 45, 3a n = 1, 4 n = 1; squamous cell Laparoscopic RH Open RH
carcinoma 76.5%, adenocarcinoma 23.5%) were treated with Number of patients 862 825
LARVH (type II n = 102, type III n = 98) (Table 1). Time taken for operation 186-344 minutes 150-310 minutes
Results: Para-aortic lymphadenectomy was performed in 170 Blood loss 225-344 ml 400-500 ml
(85%) patients and pelvic lymphadenectomy was performed in Conversion: Lap to open 1.5-25% –
all 200 patients. In 26 (13%) patients positive lymph nodes were Hospital stay 5-12 days 10-23 days
found. Major intraoperative injuries occurred in 6% of patients. Vascular injury 3-5% 0-1%
Postoperative complications occurred in 8% of patients. Bowel injury 1.5-2% 0-1%
Incidence of complications decreased significantly when Bladder injury 3.5-10% 1-1.34%
comparing the first half with the second half of patients. After a Ureteric injury 2% 2%
median follow-up time of 40 months, overall 5-year survival Postoperative 5-7% 5-20%
could be projected to 83%; 18.5% of patients experienced Infective morbidity
recurrence with 35% exclusively extrapelvic and 11% of patients Hypercarbia 0.5-1% —
died of recurrence. Independent prognostic factors for Bowel fistula 0.5-0.75% —
recurrence-free survival were tumor stage, lymph node status, Urinary fistulas 2-3% 1%
and combined involvement of lymphovascular and Disease free survival 83-94.9% 75.6-94%
angiovascular space. In the absence of these risk factors
projected 5-year survival was 98%. DISCUSSION
Conclusion: Patients with tumor < 4 cm, negative lymph nodes, Looking at the comparative analysis shown in Table 2 the
and the absence of the combination of angio- and laparoscopic radical hysterectomy with lymphadenectomy has
26
JAYPEE