Page 12 - World's Most Popular Laparoscopic Journal
P. 12
Severe Hemobilia from Hepatic Artery Pseudoaneurysm after Laparoscopic Cholecystectomy
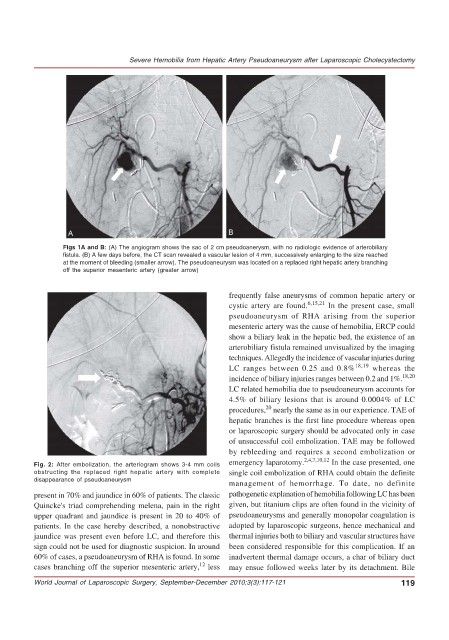
Figs 1A and B: (A) The angiogram shows the sac of 2 cm pseudoanerysm, with no radiologic evidence of arterobiliary
fistula. (B) A few days before, the CT scan revealed a vascular lesion of 4 mm, successively enlarging to the size reached
at the moment of bleeding (smaller arrow). The pseudoaneurysm was located on a replaced right hepatic artery branching
off the superior mesenteric artery (greater arrow)
frequently false aneurysms of common hepatic artery or
cystic artery are found. 6,15,21 In the present case, small
pseudoaneurysm of RHA arising from the superior
mesenteric artery was the cause of hemobilia, ERCP could
show a biliary leak in the hepatic bed, the existence of an
arterobiliary fistula remained unvisualized by the imaging
techniques. Allegedly the incidence of vascular injuries during
LC ranges between 0.25 and 0.8% 18,19 whereas the
incidence of biliary injuries ranges between 0.2 and 1%. 18,20
LC related hemobilia due to pseudoaneurysm accounts for
4.5% of biliary lesions that is around 0.0004% of LC
20
procedures, nearly the same as in our experience. TAE of
hepatic branches is the first line procedure whereas open
or laparoscopic surgery should be advocated only in case
of unsuccessful coil embolization. TAE may be followed
by rebleeding and requires a second embolization or
Fig. 2: After embolization, the arteriogram shows 3-4 mm coils emergency laparotomy. 2,4,7,10,12 In the case presented, one
obstructing the replaced right hepatic artery with complete single coil embolization of RHA could obtain the definite
disappearance of pseudoaneurysm
management of hemorrhage. To date, no definite
present in 70% and jaundice in 60% of patients. The classic pathogenetic explanation of hemobilia following LC has been
Quincke's triad comprehending melena, pain in the right given, but titanium clips are often found in the vicinity of
upper quadrant and jaundice is present in 20 to 40% of pseudoaneurysms and generally monopolar coagulation is
patients. In the case hereby described, a nonobstructive adopted by laparoscopic surgeons, hence mechanical and
jaundice was present even before LC, and therefore this thermal injuries both to biliary and vascular structures have
sign could not be used for diagnostic suspicion. In around been considered responsible for this complication. If an
60% of cases, a pseudoaneurysm of RHA is found. In some inadvertent thermal damage occurs, a char of biliary duct
12
cases branching off the superior mesenteric artery, less may ensue followed weeks later by its detachment. Bile
World Journal of Laparoscopic Surgery, September-December 2010;3(3):117-121 119