Page 10 - World's Most Popular Laparoscopic Journal
P. 10
10.5005/jp-journals-10007-1095 WJOLS
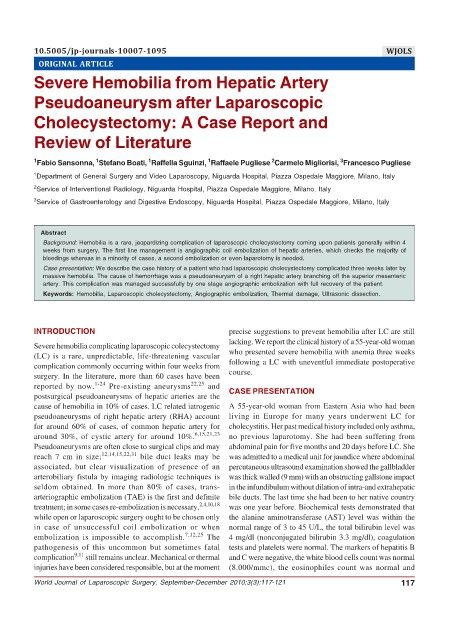
ORIGINAL ARTICLE Severe Hemobilia from Hepatic Artery Pseudoaneurysm after Laparoscopic Cholecystectomy
Severe Hemobilia from Hepatic Artery
Pseudoaneurysm after Laparoscopic
Cholecystectomy: A Case Report and
Review of Literature
3
1
1
1
2
1 Fabio Sansonna, Stefano Boati, Raffella Sguinzi, Raffaele Pugliese Carmelo Migliorisi, Francesco Pugliese
1 Department of General Surgery and Video Laparoscopy, Niguarda Hospital, Piazza Ospedale Maggiore, Milano, Italy
2 Service of Interventional Radiology, Niguarda Hospital, Piazza Ospedale Maggiore, Milano, Italy
3 Service of Gastroenterology and Digestive Endoscopy, Niguarda Hospital, Piazza Ospedale Maggiore, Milano, Italy
Abstract
Background: Hemobilia is a rare, jeopardizing complication of laparoscopic cholecystectomy coming upon patients generally within 4
weeks from surgery. The first line management is angiographic coil embolization of hepatic arteries, which checks the majority of
bleedings whereas in a minority of cases, a second embolization or even laparotomy is needed.
Case presentation: We describe the case history of a patient who had laparoscopic cholecystectomy complicated three weeks later by
massive hemobilia. The cause of hemorrhage was a pseudoaneurysm of a right hepatic artery branching off the superior mesenteric
artery. This complication was managed successfully by one stage angiographic embolization with full recovery of the patient.
Keywords: Hemobilia, Laparoscopic cholecystectomy, Angiographic embolization, Thermal damage, Ultrasonic dissection.
INTRODUCTION precise suggestions to prevent hemobilia after LC are still
lacking. We report the clinical history of a 55-year-old woman
Severe hemobilia complicating laparoscopic colecystectomy
(LC) is a rare, unpredictable, life-threatening vascular who presented severe hemobilia with anemia three weeks
complication commonly occurring within four weeks from following a LC with uneventful immediate postoperative
surgery. In the literature, more than 60 cases have been course.
reported by now. 1-24 Pre-existing aneurysms 22,25 and
postsurgical pseudoaneurysms of hepatic arteries are the CASE PRESENTATION
cause of hemobilia in 10% of cases. LC related iatrogenic A 55-year-old woman from Eastern Asia who had been
pseudoaneurysms of right hepatic artery (RHA) account living in Europe for many years underwent LC for
for around 60% of cases, of common hepatic artery for cholecystitis. Her past medical history included only asthma,
around 30%, of cystic artery for around 10%. 6,15,21,23 no previous laparotomy. She had been suffering from
Pseudoaneurysms are often close to surgical clips and may abdominal pain for five months and 20 days before LC. She
reach 7 cm in size; 12,14,15,22,31 bile duct leaks may be was admitted to a medical unit for jaundice where abdominal
associated, but clear visualization of presence of an percutaneous ultrasound examination showed the gallbladder
arterobiliary fistula by imaging radiologic techniques is was thick walled (9 mm) with an obstructing gallstone impact
seldom obtained. In more than 80% of cases, trans- in the infundibulum without dilation of intra-and extrahepatic
arteriographic embolization (TAE) is the first and definite bile ducts. The last time she had been to her native country
treatment; in some cases re-embolization is necessary, 2,4,10,18 was one year before. Biochemical tests demonstrated that
while open or laparoscopic surgery ought to be chosen only the alanine aminotransferase (AST) level was within the
in case of unsuccessful coil embolization or when normal range of 3 to 45 U/L, the total bilirubin level was
embolization is impossible to accomplish. 7,12,25 The 4 mg/dl (nonconjugated bilirubin 3.3 mg/dl), coagulation
pathogenesis of this uncommon but sometimes fatal tests and platelets were normal. The markers of hepatitis B
complication 9,11 still remains unclear. Mechanical or thermal and C were negative, the white blood cells count was normal
injuries have been considered responsible, but at the moment (8.000/mmc), the eosinophiles count was normal and
World Journal of Laparoscopic Surgery, September-December 2010;3(3):117-121 117