Page 38 - World Journal of Laparoscopic Surgery
P. 38
Laparoscopic Intervention after VP Shunt
CO2 through the peritoneal cavity and the effect of insufflation on In patients with a VP (ventriculoperitoneal) shunt, there have
ventilation can also lead to dilatation of the intracranial arteries and been concerns about performing longer laparoscopic pressure.
increases the cerebral perfusion. 5–7 In healthy people, the increased First, the general fear is based on the thought that increasing
cerebral perfusion and ICP are temporary and tend to normalize the pressure of the abdominal cavity could impair the drainage.
after 10 minutes. Second, the carbon dioxide insufflated into the abdomen could
get into the ventricular system and third, the acutely elevated ICP
and increased intracranial blood volume are caused by the elevated
8
venous pressure or hypercapnia. An acute increase in ICP may result
in a dangerous combination of hypertension with bradycardia and
subsequently a serious neurological complication as a result of a
posterior encephalic herniation (Fig. 3). 1,5–7,9
On the contrary, the presence of a foreign body, such as a VP
shunt, and the possibility of a bacterial inoculum being introduced
during the operation presumably increase the chance of developing
10
an infection and adhesions. 11–14 The direct communication
between the peritoneal cavity and the ventricular system in patients
with VP shunts could also predispose patients to developing
meningitis, shunt malformation, mental changes, seizure disorders,
and decreased intellectual abilities. 10,13–16
Patients who have VP shunts represent a special group
17
who require special attention. At the time, they have a near to
normal life expectancy and are presume to undergo laparoscopic
operations as other patients. We are presenting a case of a patient
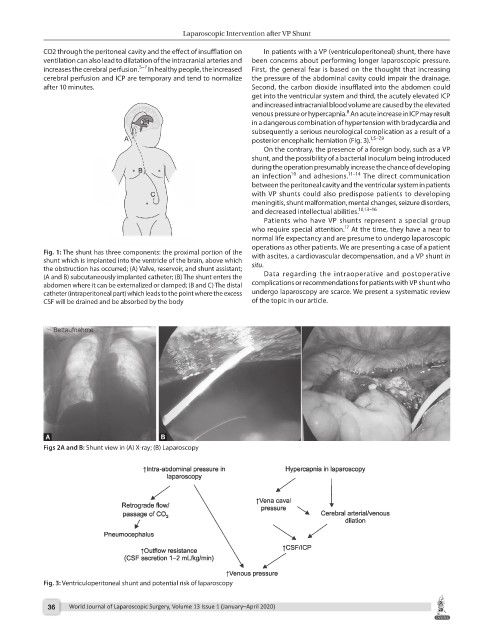
Fig. 1: The shunt has three components: the proximal portion of the with ascites, a cardiovascular decompensation, and a VP shunt in
shunt which is implanted into the ventricle of the brain, above which situ.
the obstruction has occurred; (A) Valve, reservoir, and shunt assistant;
(A and B) subcutaneously implanted catheter; (B) The shunt enters the Data regarding the intraoperative and postoperative
abdomen where it can be externalized or clamped; (B and C) The distal complications or recommendations for patients with VP shunt who
catheter (intraperitoneal part) which leads to the point where the excess undergo laparoscopy are scarce. We present a systematic review
CSF will be drained and be absorbed by the body of the topic in our article.
Figs 2A and B: Shunt view in (A) X-ray; (B) Laparoscopy
Fig. 3: Ventriculoperitoneal shunt and potential risk of laparoscopy
36 World Journal of Laparoscopic Surgery, Volume 13 Issue 1 (January–April 2020)