Page 20 - World Journal of Laparoscopic Surgery
P. 20
Hindrance to Day Care Laparoscopic Cholecystectomy in India
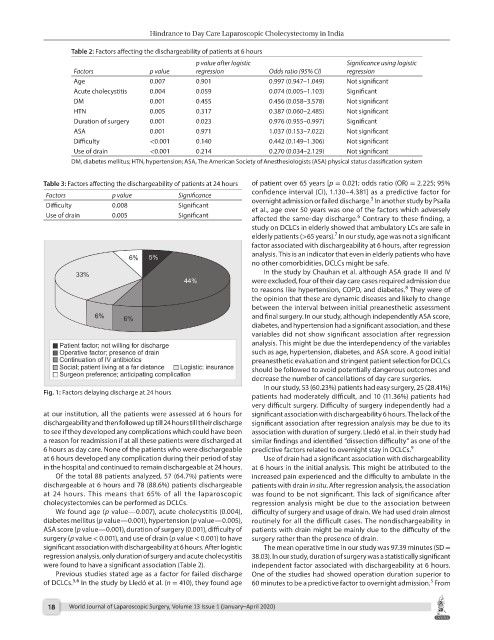
Table 2: Factors affecting the dischargeability of patients at 6 hours
p value after logistic Significance using logistic
Factors p value regression Odds ratio (95% CI) regression
Age 0.007 0.901 0.997 (0.947–1.049) Not significant
Acute cholecystitis 0.004 0.059 0.074 (0.005–1.103) Significant
DM 0.001 0.455 0.456 (0.058–3.578) Not significant
HTN 0.005 0.317 0.387 (0.060–2.485) Not significant
Duration of surgery 0.001 0.023 0.976 (0.955–0.997) Significant
ASA 0.001 0.971 1.037 (0.153–7.022) Not significant
Difficulty <0.001 0.140 0.442 (0.149–1.306) Not significant
Use of drain <0.001 0.214 0.270 (0.034–2.129) Not significant
DM, diabetes mellitus; HTN, hypertension; ASA, The American Society of Anesthesiologists (ASA) physical status classification system
Table 3: Factors affecting the dischargeability of patients at 24 hours of patient over 65 years [p = 0.021; odds ratio (OR) = 2.225; 95%
Factors p value Significance confidence interval (CI), 1.130–4.381] as a predictive factor for
5
Difficulty 0.008 Significant overnight admission or failed discharge. In another study by Psaila
et al., age over 50 years was one of the factors which adversely
Use of drain 0.005 Significant 6
affected the same-day discharge. Contrary to these finding, a
study on DCLCs in elderly showed that ambulatory LCs are safe in
7
elderly patients (>65 years). In our study, age was not a significant
factor associated with dischargeability at 6 hours, after regression
analysis. This is an indicator that even in elderly patients who have
no other comorbidities, DCLCs might be safe.
In the study by Chauhan et al. although ASA grade III and IV
were excluded, four of their day care cases required admission due
8
to reasons like hypertension, COPD, and diabetes. They were of
the opinion that these are dynamic diseases and likely to change
between the interval between initial preanesthetic assessment
and final surgery. In our study, although independently ASA score,
diabetes, and hypertension had a significant association, and these
variables did not show significant association after regression
analysis. This might be due the interdependency of the variables
such as age, hypertension, diabetes, and ASA score. A good initial
preanesthetic evaluation and stringent patient selection for DCLCs
should be followed to avoid potentially dangerous outcomes and
decrease the number of cancellations of day care surgeries.
In our study, 53 (60.23%) patients had easy surgery, 25 (28.41%)
Fig. 1: Factors delaying discharge at 24 hours
patients had moderately difficult, and 10 (11.36%) patients had
very difficult surgery. Difficulty of surgery independently had a
at our institution, all the patients were assessed at 6 hours for significant association with dischargeability 6 hours. The lack of the
dischargeability and then followed up till 24 hours till their discharge significant association after regression analysis may be due to its
to see if they developed any complications which could have been association with duration of surgery. Lledó et al. in their study had
a reason for readmission if at all these patients were discharged at similar findings and identified “dissection difficulty” as one of the
6 hours as day care. None of the patients who were dischargeable predictive factors related to overnight stay in DCLCs. 9
at 6 hours developed any complication during their period of stay Use of drain had a significant association with dischargeability
in the hospital and continued to remain dischargeable at 24 hours. at 6 hours in the initial analysis. This might be attributed to the
Of the total 88 patients analyzed, 57 (64.7%) patients were increased pain experienced and the difficulty to ambulate in the
dischargeable at 6 hours and 78 (88.6%) patients dischargeable patients with drain in situ. After regression analysis, the association
at 24 hours. This means that 65% of all the laparoscopic was found to be not significant. This lack of significance after
cholecystectomies can be performed as DCLCs. regression analysis might be due to the association between
We found age (p value—0.007), acute cholecystitis (0.004), difficulty of surgery and usage of drain. We had used drain almost
diabetes mellitus (p value—0.001), hypertension (p value—0.005), routinely for all the difficult cases. The nondischargeability in
ASA score (p value—0.001), duration of surgery (0.001), difficulty of patients with drain might be mainly due to the difficulty of the
surgery (p value < 0.001), and use of drain (p value < 0.001) to have surgery rather than the presence of drain.
significant association with dischargeability at 6 hours. After logistic The mean operative time in our study was 97.39 minutes (SD =
regression analysis, only duration of surgery and acute cholecystitis 38.03). In our study, duration of surgery was a statistically significant
were found to have a significant association (Table 2). independent factor associated with dischargeability at 6 hours.
Previous studies stated age as a factor for failed discharge One of the studies had showed operation duration superior to
5,6
5
of DCLCs. In the study by Lledó et al. (n = 410), they found age 60 minutes to be a predictive factor to overnight admission. From
18 World Journal of Laparoscopic Surgery, Volume 13 Issue 1 (January–April 2020)