Page 25 - World Journal of Laparoscopic Surgery
P. 25
Mini Two-port Laparoscopic Appendicectomy with Novel Knotting Technique
Better cosmesis achieved in TPA as scar was hidden in umbilicus occurrence leads to many difficulties in diagnosis. Diagnosis
and pubic hairline producing scarless appearance (Fig. 4) and scar of acute appendicitis includes clinical examination, laboratory
was visible at umbilicus and left iliac fossa in CLA. Infection rate tests, diagnostic scoring systems, and imaging modalities like
was 0.59% and 3.125% for TPA and CLA, respectively. Incidence of ultrasonography and computerized tomography. CT demonstrates
5
intraoperative bleeding and intraoperative rupture of appendix a sensitivity and specificity of 83%–100%. Scoring systems link
was less in TPA (1.19% and 0%, respectively) as compared to CLA clinical examination and laboratory tests by certain quantification
(6.25% and 3.125%, respectively). Mean hospital stay was less in of symptoms, signs, and laboratory parameters. 6
TPA (1.7 days) compared to CLA (2.1 days). No major intraoperative The first successful appendicectomy was performed in by
complications were observed (Table 1). Claudius Amyand in 1735. Laparoscopic appendicectomy was first
7
performed by the German gynecologist Kurt Semm in 1980, which
dIscussIon became a new gold standard in surgical treatment of appendicitis.
8
1
The incidence of appendicitis gradually rises from birth, peaks in Surgical advancement in the management of acute appendicitis
2
the late 10 years, and gradually declines in the geriatric years. It has evolved in great extent in the last 120 years, from McBurney’s
is most prevalent in young belonging to the age group of 10–19 simple large incision and its modification to minimally invasive LA,
3
years. In recent years, the number of cases in patients aged 30–69 to barely noticeable incisions after single-incision laparoscopic
4
years has increased to 6.3%. However, cosmesis has been an utmost surgery (SILS). 9
importance lately among all the age groups. The safest treatment in all stages of the inflamed appendix
10
Clinical presentation of 30% to 45% patients suspected of is appendicectomy. Open appendicectomy always results in a
appendicitis is frequently unspecified and despite common disfiguring scar over the abdomen. Cosmetic outcome is important
to consider as the disease affects mainly the young people. 11,12 Apart
13
from cosmesis, Larson et al. has established numerous reasons
why a laparoscopic procedure stands superior to the conventional
open appendicectomy which includes better visualization and
magnification, exploration of all surrounding viscera, better
handling in obese patients, minimal tissue trauma, and reduced
the incidence of surgical-site infection. 14,15
The conventional three-port laparoscopic appendicectomy
includes 10-mm camera port at the umbilicus and 2 working 5-mm
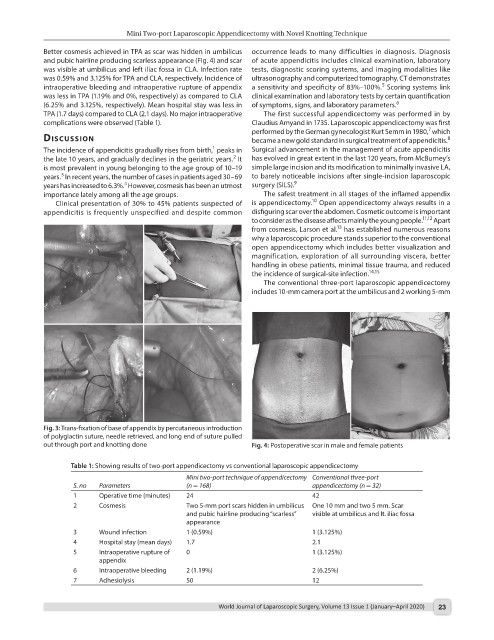
Fig. 3: Trans-fixation of base of appendix by percutaneous introduction
of polyglactin suture, needle retrieved, and long end of suture pulled
out through port and knotting done Fig. 4: Postoperative scar in male and female patients
Table 1: Showing results of two-port appendicectomy vs conventional laparoscopic appendicectomy
Mini two-port technique of appendicectomy Conventional three-port
S. no Parameters (n = 168) appendicectomy (n = 32)
1 Operative time (minutes) 24 42
2 Cosmesis Two 5-mm port scars hidden in umbilicus One 10 mm and two 5 mm. Scar
and pubic hairline producing “scarless” visible at umbilicus and lt. iliac fossa
appearance
3 Wound infection 1 (0.59%) 1 (3.125%)
4 Hospital stay (mean days) 1.7 2.1
5 Intraoperative rupture of 0 1 (3.125%)
appendix
6 Intraoperative bleeding 2 (1.19%) 2 (6.25%)
7 Adhesiolysis 50 12
World Journal of Laparoscopic Surgery, Volume 13 Issue 1 (January–April 2020) 23