Page 15 - World Journal of Laparoscopic Surgery
P. 15
Drainage of Complex Pyogenic Liver Abscess
was irrigated by normal saline, and proper hemostasis was secured. results
Finally, an abdominal drain was placed in the abscess cavity and
another one in the pelvis (Fig. 3). Forty-eight patients (20 males and 28 females) with a median age
of 54.5 years (ranges between 34 years and 65 years) were included
Open Surgery in this study. The clinical and laboratory data of patients with CPLA
A right subcostal incision or a midline abdominal incision was made at presentation are shown in Table 1.
according to abscess location. Intraoperative ultrasound was done All patient were diagnosed by one or two imaging modalities
to detect the exact site and extent of the liver abscess then de (ultrasonography, CT, or MRI) and all were successfully treated either
roofing of the abscess to drain pus and remove the fibrous septa. by laparoscopic drainage or open surgery confirmed by at least one
Hemostasis was secured and latex drainage tube was left (Fig. 2). image modality, CT or MRI examination (Figs 4 and 5).
Operative and clinical data including operation time, All patients received broad spectrum antibiotics. Nine
intraoperative blood loss, postoperative complication rate, length patients had preoperative failed trial of percutaneous drainage.
of postoperative hospital stay, and rate of abscess recurrence were Twenty-six patients were managed by open surgical drainage
compared between the two groups. and 22 patients by laparoscopic drainage. The operation time
Regular follow-up was done weekly for the first month and hospital stay were less and oral feeding was started earlier
after discharge then every 2 months for about one year. Clinical in laparoscopic drainage group. Wound infection was higher
examination and abdominal ultrasound were done every visit. in open drainage group. Abscess recurrence occurred once
in laparoscopic group and once in open surgery group and
Study Design both were successfully treated with percutaneous drainage.
Combined retrospective and prospective study of all complex liver One laparoscopic operation was converted into open surgical
abscesses admitted to NHTMRI from January 2012 to January 2020 drainage due to unsatisfactory laparoscopic drainage. Results
and comparison between laparoscopic and open surgical drainage are shown in Table 2.
as regards safety, efficacy, hospital stay, perioperative morbidity, In pus-culture study of the 48 patients, only 38 cases (79%) had
mortality, and recurrence. positive microbial reports while 21% had reports with no growth.
Table 1: Clinical and laboratory data of patients with complex pyogenic
liver abscess at presentation
Variables LD group (n = 22) OSD group (n = 26)
Abdominal pain 21 25
Fever/rigors 21 26
Vomiting 11 12
Jaundice 5 6
Abdominal tenderness 19 23
Severe sepsis 1 8
Leukocytosis (>11,000/mL) 22 26
Elevated AST/ALT 12 15
Serum albumin (<3.5 g/dL) 7 9
Total bilirubin (>2 mg/dL) 6 9
Serum creatinine 1 8
(>1.4 mg/dL)
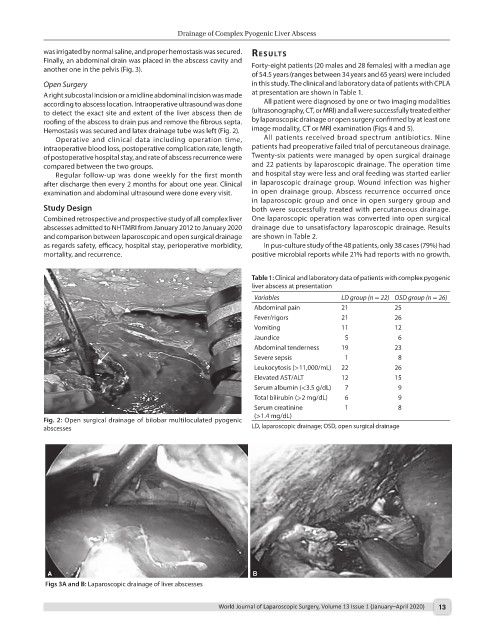
Fig. 2: Open surgical drainage of bilobar multiloculated pyogenic
abscesses LD, laparoscopic drainage; OSD, open surgical drainage
Figs 3A and B: Laparoscopic drainage of liver abscesses
World Journal of Laparoscopic Surgery, Volume 13 Issue 1 (January–April 2020) 13