Page 10 - World Journal of Laparoscopic Surgery
P. 10
Laparoscopic Common Bile Duct Exploration
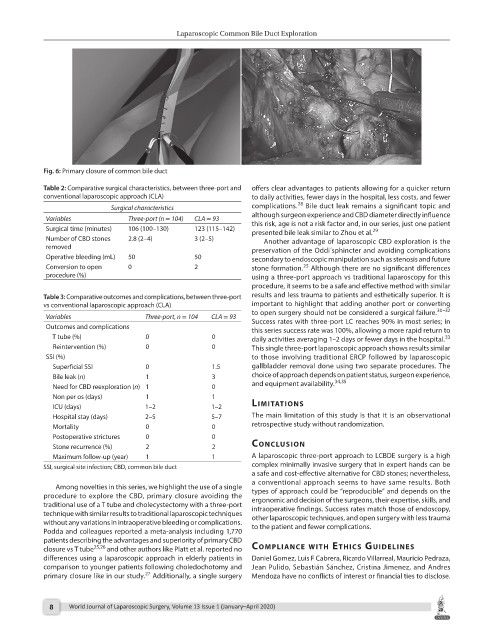
Fig. 6: Primary closure of common bile duct
Table 2: Comparative surgical characteristics, between three-port and offers clear advantages to patients allowing for a quicker return
conventional laparoscopic approach (CLA) to daily activities, fewer days in the hospital, less costs, and fewer
28
Surgical characteristics complications. Bile duct leak remains a significant topic and
Variables Three-port (n = 104) CLA = 93 although surgeon experience and CBD diameter directly influence
this risk, age is not a risk factor and, in our series, just one patient
Surgical time (minutes) 106 (100–130) 123 (115–142) presented bile leak similar to Zhou et al. 29
Number of CBD stones 2.8 (2–4) 3 (2–5) Another advantage of laparoscopic CBD exploration is the
removed preservation of the Oddi´sphincter and avoiding complications
Operative bleeding (mL) 50 50 secondary to endoscopic manipulation such as stenosis and future
Conversion to open 0 2 stone formation. Although there are no significant differences
25
procedure (%) using a three-port approach vs traditional laparoscopy for this
procedure, it seems to be a safe and effective method with similar
Table 3: Comparative outcomes and complications, between three-port results and less trauma to patients and esthetically superior. It is
vs conventional laparoscopic approach (CLA) important to highlight that adding another port or converting
to open surgery should not be considered a surgical failure. 30–32
Variables Three-port, n = 104 CLA = 93 Success rates with three-port LC reaches 90% in most series; in
Outcomes and complications this series success rate was 100%, allowing a more rapid return to
T tube (%) 0 0 daily activities averaging 1–2 days or fewer days in the hospital.
33
Reintervention (%) 0 0 This single three-port laparoscopic approach shows results similar
SSI (%) to those involving traditional ERCP followed by laparoscopic
Superficial SSI 0 1.5 gallbladder removal done using two separate procedures. The
Bile leak (n) 1 3 choice of approach depends on patient status, surgeon experience,
34,35
Need for CBD reexploration (n) 1 0 and equipment availability.
Non per os (days) 1 1 lIMItAtIons
ICU (days) 1–2 1–2
Hospital stay (days) 2–5 5–7 The main limitation of this study is that it is an observational
Mortality 0 0 retrospective study without randomization.
Postoperative strictures 0 0
Stone recurrence (%) 2 2 conclusIon
Maximum follow-up (year) 1 1 A laparoscopic three-port approach to LCBDE surgery is a high
SSI, surgical site infection; CBD, common bile duct complex minimally invasive surgery that in expert hands can be
a safe and cost-effective alternative for CBD stones; nevertheless,
a conventional approach seems to have same results. Both
Among novelties in this series, we highlight the use of a single types of approach could be “reproducible” and depends on the
procedure to explore the CBD, primary closure avoiding the ergonomic and decision of the surgeons, their expertise, skills, and
traditional use of a T tube and cholecystectomy with a three-port intraoperative findings. Success rates match those of endoscopy,
technique with similar results to traditional laparoscopic techniques other laparoscopic techniques, and open surgery with less trauma
without any variations in intraoperative bleeding or complications. to the patient and fewer complications.
Podda and colleagues reported a meta-analysis including 1,770
patients describing the advantages and superiority of primary CBD
closure vs T tube 25,26 and other authors like Platt et al. reported no coMplIAnce wIth ethIcs guIdelInes
differences using a laparoscopic approach in elderly patients in Daniel Gomez, Luis F Cabrera, Ricardo Villarreal, Mauricio Pedraza,
comparison to younger patients following choledochotomy and Jean Pulido, Sebastián Sánchez, Cristina Jimenez, and Andres
27
primary closure like in our study. Additionally, a single surgery Mendoza have no conflicts of interest or financial ties to disclose.
8 World Journal of Laparoscopic Surgery, Volume 13 Issue 1 (January–April 2020)