Page 12 - Journal of Laparoscopic Surgery - WALS Journal
P. 12
Apoorv Goel et al
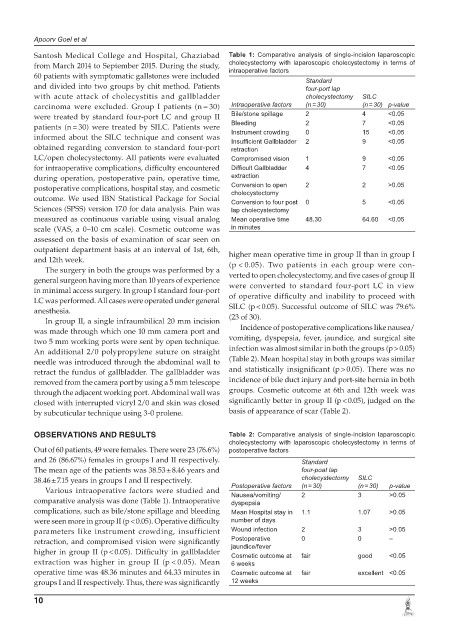
Santosh Medical College and Hospital, Ghaziabad Table 1: Comparative analysis of single-incision laparoscopic
from March 2014 to September 2015. During the study, cholecystectomy with laparoscopic cholecystectomy in terms of
intraoperative factors
60 patients with symptomatic gallstones were included Standard
and divided into two groups by chit method. Patients four-port lap
with acute attack of cholecystitis and gallbladder cholecystectomy SILC
carcinoma were excluded. Group I patients (n = 30) Intraoperative factors (n = 30) (n = 30) p-value
were treated by standard four-port LC and group II Bile/stone spillage 2 4 <0.05
patients (n = 30) were treated by SILC. Patients were Bleeding 2 7 <0.05
15
0
Instrument crowding
<0.05
informed about the SILC technique and consent was Insufficient Gallbladder 2 9 <0.05
obtained regarding conversion to standard four-port retraction
LC/open cholecystectomy. All patients were evaluated Compromised vision 1 9 <0.05
for intraoperative complications, difficulty encountered Difficult Gallbladder 4 7 <0.05
during operation, postoperative pain, operative time, extraction
postoperative complications, hospital stay, and cosmetic Conversion to open 2 2 >0.05
cholecystectomy
outcome. We used IBN Statistical Package for Social Conversion to four post 0 5 <0.05
Sciences (SPSS) version 17.0 for data analysis. Pain was lap cholecystectomy
measured as continuous variable using visual analog Mean operative time 48.30 64.60 <0.05
scale (VAS, a 0–10 cm scale). Cosmetic outcome was in minutes
assessed on the basis of examination of scar seen on
outpatient department basis at an interval of 1st, 6th, higher mean operative time in group II than in group I
and 12th week. (p < 0.05). Two patients in each group were con-
The surgery in both the groups was performed by a
general surgeon having more than 10 years of experience verted to open cholecystectomy, and five cases of group II
in minimal access surgery. In group I standard four-port were converted to standard four-port LC in view
LC was performed. All cases were operated under general of operative difficulty and inability to proceed with
anesthesia. SILC (p < 0.05). Successful outcome of SILC was 79.6%
In group II, a single infraumbilical 20 mm incision (23 of 30).
was made through which one 10 mm camera port and Incidence of postoperative complications like nausea/
two 5 mm working ports were sent by open technique. vomiting, dyspepsia, fever, jaundice, and surgical site
An additional 2/0 polypropylene suture on straight infection was almost similar in both the groups (p > 0.05)
needle was introduced through the abdominal wall to (Table 2). Mean hospital stay in both groups was similar
retract the fundus of gallbladder. The gallbladder was and statistically insignificant (p > 0.05). There was no
removed from the camera port by using a 5 mm telescope incidence of bile duct injury and port-site hernia in both
through the adjacent working port. Abdominal wall was groups. Cosmetic outcome at 6th and 12th week was
closed with interrupted vicryl 2/0 and skin was closed significantly better in group II (p < 0.05), judged on the
by subcuticular technique using 3-0 prolene. basis of appearance of scar (Table 2).
OBSERVATIONS AND RESULTS Table 2: Comparative analysis of single-incision laparoscopic
cholecystectomy with laparoscopic cholecystectomy in terms of
Out of 60 patients, 49 were females. There were 23 (76.6%) postoperative factors
and 26 (86.67%) females in groups I and II respectively. Standard
The mean age of the patients was 38.53 ± 8.46 years and four-poat lap
38.46 ± 7.15 years in groups I and II respectively. cholecystectomy SILC
Various intraoperative factors were studied and Postoperative factors (n = 30) (n = 30) p-value
2
Nausea/vomiting/
>0.05
3
comparative analysis was done (Table 1). Intraoperative dyspepsia
complications, such as bile/stone spillage and bleeding Mean Hospital stay in 1.1 1.07 >0.05
were seen more in group II (p < 0.05). Operative difficulty number of days
parameters like instrument crowding, insufficient Wound infection 2 3 >0.05
retraction, and compromised vision were significantly Postoperative 0 0 –
jaundice/fever
higher in group II (p < 0.05). Difficulty in gallbladder Cosmetic outcome at fair good <0.05
extraction was higher in group II (p < 0.05). Mean 6 weeks
operative time was 48.36 minutes and 64.33 minutes in Cosmetic outcome at fair excellent <0.05
groups I and II respectively. Thus, there was significantly 12 weeks
10