Page 8 - Journal of Laparoscopic Surgery - WALS Journal
P. 8
Ankush Jairath et al
comorbidity, and those needing conversion to open using Student’s t test. Epi Info statistical software was
cholecystectomy were excluded from the study. used for all analyses.
After preoxygenation with 100% oxygen for 3 minutes,
induction of anesthesia was achieved with thiopentone ReSULTS
sodium (2.5%) 4 to 6 mg/kg intravenous (IV) slowly (till For this study, 100 patients were recruited. There were no
the abolition of eye lash reflex) along with injection of significant differences between two groups according to
fentanyl 1.5 μg/kg IV. Intubation is with an appropriate age, sex, and body weight (Table 1).
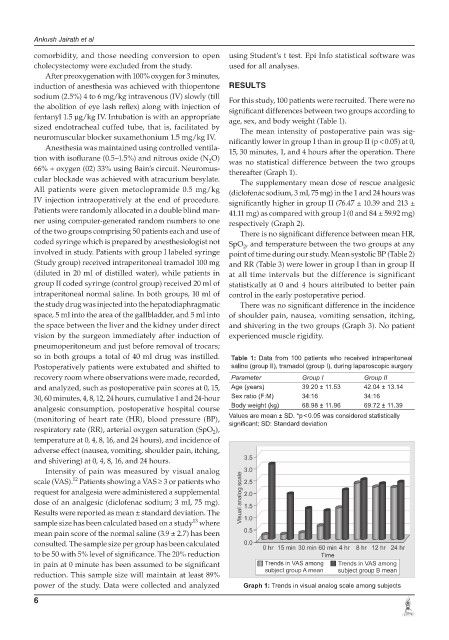
sized endotracheal cuffed tube, that is, facilitated by The mean intensity of postoperative pain was sig-
neuromuscular blocker suxamethonium 1.5 mg/kg IV. nificantly lower in group I than in group II (p < 0.05) at 0,
Anesthesia was maintained using controlled ventila- 15, 30 minutes, 1, and 4 hours after the operation. There
tion with isoflurane (0.5–1.5%) and nitrous oxide (N O) was no statistical difference between the two groups
2
66% + oxygen (02) 33% using Bain’s circuit. Neuromus- thereafter (Graph 1).
cular blockade was achieved with atracurium besylate. The supplementary mean dose of rescue analgesic
All patients were given metoclopramide 0.5 mg/kg (diclofenac sodium, 3 ml, 75 mg) in the 1 and 24 hours was
IV injection intraoperatively at the end of procedure. significantly higher in group II (76.47 ± 10.39 and 213 ±
Patients were randomly allocated in a double blind man- 41.11 mg) as compared with group I (0 and 84 ± 59.92 mg)
ner using computer-generated random numbers to one respectively (Graph 2).
of the two groups comprising 50 patients each and use of There is no significant difference between mean HR,
coded syringe which is prepared by anesthesiologist not SpO , and temperature between the two groups at any
2
involved in study. Patients with group I labeled syringe point of time during our study. Mean systolic BP (Table 2)
(Study group) received intraperitoneal tramadol 100 mg and RR (Table 3) were lower in group I than in group II
(diluted in 20 ml of distilled water), while patients in at all time intervals but the difference is significant
group II coded syringe (control group) received 20 ml of statistically at 0 and 4 hours attributed to better pain
intraperitoneal normal saline. In both groups, 10 ml of control in the early postoperative period.
the study drug was injected into the hepatodiaphragmatic There was no significant difference in the incidence
space, 5 ml into the area of the gallbladder, and 5 ml into of shoulder pain, nausea, vomiting sensation, itching,
the space between the liver and the kidney under direct and shivering in the two groups (Graph 3). No patient
vision by the surgeon immediately after induction of experienced muscle rigidity.
pneumoperitoneum and just before removal of trocars;
so in both groups a total of 40 ml drug was instilled. Table 1: Data from 100 patients who received intraperitoneal
Postoperatively patients were extubated and shifted to saline (group II), tramadol (group I), during laparoscopic surgery
recovery room where observations were made, recorded, Parameter Group I Group II
and analyzed, such as postoperative pain scores at 0, 15, Age (years) 39.20 ± 11.53 42.04 ± 13.14
30, 60 minutes, 4, 8, 12, 24 hours, cumulative 1 and 24-hour Sex ratio (F:M) 34:16 34:16
analgesic consumption, postoperative hospital course Body weight (kg) 68.98 ± 11.96 69.72 ± 11.39
(monitoring of heart rate (HR), blood pressure (BP), Values are mean ± SD. *p < 0.05 was considered statistically
significant; SD: Standard deviation
respiratory rate (RR), arterial oxygen saturation (SpO ),
2
temperature at 0, 4, 8, 16, and 24 hours), and incidence of
adverse effect (nausea, vomiting, shoulder pain, itching,
and shivering) at 0, 4, 8, 16, and 24 hours.
Intensity of pain was measured by visual analog
12
scale (VAS). Patients showing a VAS ≥ 3 or patients who
request for analgesia were administered a supplemental
dose of an analgesic (diclofenac sodium; 3 ml, 75 mg).
Results were reported as mean ± standard deviation. The
13
sample size has been calculated based on a study where
mean pain score of the normal saline (3.9 ± 2.7) has been
consulted. The sample size per group has been calculated
to be 50 with 5% level of significance. The 20% reduction
in pain at 0 minute has been assumed to be significant
reduction. This sample size will maintain at least 89%
power of the study. Data were collected and analyzed Graph 1: Trends in visual analog scale among subjects
6