Laparoscopic Treatment of Rectal Prolapse
Laparoscopic Treatment of Rectal Prolapse: A Minimally Invasive Solution for a Complex Condition
Introduction
Rectal prolapse is a distressing medical condition characterized by the protrusion of the rectum through the anus. It can significantly impact a patient's quality of life, causing discomfort, embarrassment, and functional impairment. While rectal prolapse can be managed through various surgical and non-surgical approaches, this article focuses on the innovative and minimally invasive technique of laparoscopic treatment.
Understanding Rectal Prolapse
Before delving into the laparoscopic approach, it's essential to understand rectal prolapse itself. Rectal prolapse occurs when the rectum, the lower part of the large intestine, loses its normal attachments inside the body and protrudes outside the anal opening. This condition is more common in elderly individuals, females, and those with a history of chronic constipation or childbirth trauma.
Rectal prolapse can manifest in three distinct forms:
1. Mucosal Prolapse: Only the inner lining of the rectum (mucosa) protrudes through the anus.
2. Partial Prolapse: A portion of the rectal wall extends outside the anal opening.
3. Complete Prolapse: The entire thickness of the rectal wall is everted through the anus.
The symptoms of rectal prolapse can range from mild discomfort and incontinence to severe pain and fecal incontinence. Traditional surgical treatments, such as abdominal or perineal approaches, have been used for years, but laparoscopic surgery has emerged as a promising alternative.
The Laparoscopic Advantage
Laparoscopic surgery, also known as minimally invasive surgery, is a technique that offers several advantages over traditional open surgery:
1. Smaller Incisions: Laparoscopic procedures involve tiny incisions compared to the large incisions required in open surgery. This reduces the risk of infection, minimizes scarring, and accelerates postoperative recovery.
2. Improved Visualization: Surgeons use a laparoscope, a long, thin tube with a camera, to view the surgical site in high-definition on a monitor. This provides enhanced visibility and precision during the procedure.
3. Less Pain: Smaller incisions and less tissue disruption result in reduced postoperative pain and the need for fewer pain medications.
4. Shorter Hospital Stays: Patients typically spend less time in the hospital following laparoscopic surgery, leading to faster overall recovery.
The Laparoscopic Procedure for Rectal Prolapse
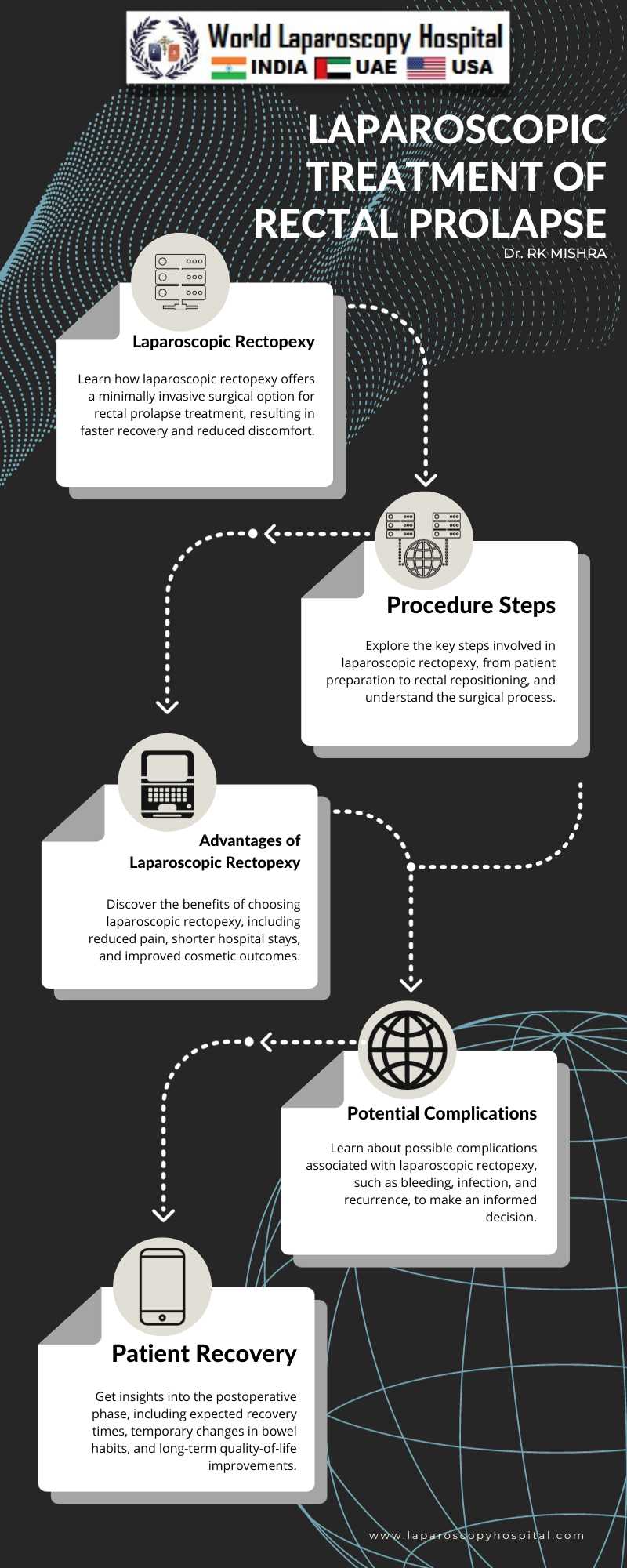
Laparoscopic treatment of rectal prolapse, often referred to as laparoscopic rectopexy, is gaining popularity among surgeons and patients alike. The procedure involves the following key steps:
1. Patient Preparation: The patient is placed under general anesthesia to ensure comfort and unconsciousness throughout the surgery.
2. Trocar Placement: The surgeon makes a few small incisions in the abdominal wall, through which trocars (thin tubes) are inserted. These serve as entry points for surgical instruments and the laparoscope.
3. Rectopexy: Using the laparoscope and specialized instruments, the surgeon carefully lifts the rectum into its normal position within the pelvis. This is achieved by reattaching the rectum to the surrounding structures, such as the sacrum, to prevent future prolapse.
4. Mesh Application (Optional): In some cases, a synthetic mesh may be placed to provide additional support to the rectum, reducing the risk of recurrence.
5. Closure and Recovery: Once the procedure is complete, the trocars are removed, and the small incisions are closed with sutures or staples. The patient is then closely monitored during the recovery phase.
Advancements in Laparoscopic Rectopexy
Recent advancements in laparoscopic rectopexy techniques have further improved patient outcomes. These include:
1. Robotic-Assisted Laparoscopic Surgery: Robotic surgical systems offer enhanced dexterity and precision, making them valuable tools in laparoscopic rectal prolapse repair.
2. Tailored Approaches: Surgeons can tailor the procedure to the patient's specific condition, ensuring personalized treatment.
3. Enhanced Mesh Technologies: The development of innovative mesh materials has led to improved long-term results and reduced complications.
Benefits and Outcomes
Laparoscopic treatment of rectal prolapse offers numerous benefits:
1. Faster Recovery: Patients often return to their normal activities more quickly than with open surgery.
2. Reduced Pain: Postoperative pain is typically minimal, requiring less pain medication.
3. Lower Infection Risk: Smaller incisions reduce the risk of surgical site infections.
4. Improved Cosmetic Result: Smaller scars are more cosmetically appealing.
5. Enhanced Quality of Life: Many patients experience relief from the discomfort and embarrassment associated with rectal prolapse.
Potential Complications
While laparoscopic rectopexy is generally considered safe, it's essential to be aware of potential complications, which may include:
1. Bleeding: Excessive bleeding during or after the procedure can occur.
2. Infection: As with any surgery, there is a risk of infection, although it is relatively low in laparoscopic procedures.
3. Recurrence: While laparoscopic rectopexy has a low recurrence rate, it is not entirely risk-free.
4. Bowel Dysfunction: Some patients may experience temporary changes in bowel habits following surgery.
5. Mesh-related Issues: Complications related to mesh, such as erosion or infection, are possible.
Conclusion
Laparoscopic treatment of rectal prolapse represents a significant advancement in the management of this complex condition. It offers patients a less invasive option with faster recovery times, reduced pain, and improved cosmetic results. While no surgery is without risks, laparoscopic rectopexy has demonstrated favorable outcomes for many individuals suffering from rectal prolapse. As technology and techniques continue to evolve, it is likely that this approach will become even more refined and widely adopted, ultimately improving the lives of those affected by rectal prolapse. Patients considering this procedure should consult with a qualified surgeon to discuss their individual case and potential treatment options.
Introduction
Rectal prolapse is a distressing medical condition characterized by the protrusion of the rectum through the anus. It can significantly impact a patient's quality of life, causing discomfort, embarrassment, and functional impairment. While rectal prolapse can be managed through various surgical and non-surgical approaches, this article focuses on the innovative and minimally invasive technique of laparoscopic treatment.
Understanding Rectal Prolapse
Before delving into the laparoscopic approach, it's essential to understand rectal prolapse itself. Rectal prolapse occurs when the rectum, the lower part of the large intestine, loses its normal attachments inside the body and protrudes outside the anal opening. This condition is more common in elderly individuals, females, and those with a history of chronic constipation or childbirth trauma.
Rectal prolapse can manifest in three distinct forms:
1. Mucosal Prolapse: Only the inner lining of the rectum (mucosa) protrudes through the anus.
2. Partial Prolapse: A portion of the rectal wall extends outside the anal opening.
3. Complete Prolapse: The entire thickness of the rectal wall is everted through the anus.
The symptoms of rectal prolapse can range from mild discomfort and incontinence to severe pain and fecal incontinence. Traditional surgical treatments, such as abdominal or perineal approaches, have been used for years, but laparoscopic surgery has emerged as a promising alternative.
The Laparoscopic Advantage
Laparoscopic surgery, also known as minimally invasive surgery, is a technique that offers several advantages over traditional open surgery:
1. Smaller Incisions: Laparoscopic procedures involve tiny incisions compared to the large incisions required in open surgery. This reduces the risk of infection, minimizes scarring, and accelerates postoperative recovery.
2. Improved Visualization: Surgeons use a laparoscope, a long, thin tube with a camera, to view the surgical site in high-definition on a monitor. This provides enhanced visibility and precision during the procedure.
3. Less Pain: Smaller incisions and less tissue disruption result in reduced postoperative pain and the need for fewer pain medications.
4. Shorter Hospital Stays: Patients typically spend less time in the hospital following laparoscopic surgery, leading to faster overall recovery.
The Laparoscopic Procedure for Rectal Prolapse
Laparoscopic treatment of rectal prolapse, often referred to as laparoscopic rectopexy, is gaining popularity among surgeons and patients alike. The procedure involves the following key steps:
1. Patient Preparation: The patient is placed under general anesthesia to ensure comfort and unconsciousness throughout the surgery.
2. Trocar Placement: The surgeon makes a few small incisions in the abdominal wall, through which trocars (thin tubes) are inserted. These serve as entry points for surgical instruments and the laparoscope.
3. Rectopexy: Using the laparoscope and specialized instruments, the surgeon carefully lifts the rectum into its normal position within the pelvis. This is achieved by reattaching the rectum to the surrounding structures, such as the sacrum, to prevent future prolapse.
4. Mesh Application (Optional): In some cases, a synthetic mesh may be placed to provide additional support to the rectum, reducing the risk of recurrence.
5. Closure and Recovery: Once the procedure is complete, the trocars are removed, and the small incisions are closed with sutures or staples. The patient is then closely monitored during the recovery phase.
Advancements in Laparoscopic Rectopexy
Recent advancements in laparoscopic rectopexy techniques have further improved patient outcomes. These include:
1. Robotic-Assisted Laparoscopic Surgery: Robotic surgical systems offer enhanced dexterity and precision, making them valuable tools in laparoscopic rectal prolapse repair.
2. Tailored Approaches: Surgeons can tailor the procedure to the patient's specific condition, ensuring personalized treatment.
3. Enhanced Mesh Technologies: The development of innovative mesh materials has led to improved long-term results and reduced complications.
Benefits and Outcomes
Laparoscopic treatment of rectal prolapse offers numerous benefits:
1. Faster Recovery: Patients often return to their normal activities more quickly than with open surgery.
2. Reduced Pain: Postoperative pain is typically minimal, requiring less pain medication.
3. Lower Infection Risk: Smaller incisions reduce the risk of surgical site infections.
4. Improved Cosmetic Result: Smaller scars are more cosmetically appealing.
5. Enhanced Quality of Life: Many patients experience relief from the discomfort and embarrassment associated with rectal prolapse.
Potential Complications
While laparoscopic rectopexy is generally considered safe, it's essential to be aware of potential complications, which may include:
1. Bleeding: Excessive bleeding during or after the procedure can occur.
2. Infection: As with any surgery, there is a risk of infection, although it is relatively low in laparoscopic procedures.
3. Recurrence: While laparoscopic rectopexy has a low recurrence rate, it is not entirely risk-free.
4. Bowel Dysfunction: Some patients may experience temporary changes in bowel habits following surgery.
5. Mesh-related Issues: Complications related to mesh, such as erosion or infection, are possible.
Conclusion
Laparoscopic treatment of rectal prolapse represents a significant advancement in the management of this complex condition. It offers patients a less invasive option with faster recovery times, reduced pain, and improved cosmetic results. While no surgery is without risks, laparoscopic rectopexy has demonstrated favorable outcomes for many individuals suffering from rectal prolapse. As technology and techniques continue to evolve, it is likely that this approach will become even more refined and widely adopted, ultimately improving the lives of those affected by rectal prolapse. Patients considering this procedure should consult with a qualified surgeon to discuss their individual case and potential treatment options.
1 COMMENTS
Dr. B S Gautam
#1
Nov 26th, 2023 9:06 am
Rectal prolapse, a distressing condition impacting quality of life, finds relief through innovative laparoscopic treatment. This minimally invasive technique addresses discomfort, embarrassment, and functional impairment, offering a comprehensive solution in this enlightening article.
| Older Post | Home | Newer Post |





