Sleeve-plus procedures offer a host of advantages that make them a compelling choice in the realm of bariatric surgery. These techniques not only serve as effective weight-loss solutions but also come with several key benefits that set them apart from other surgical options.
**1. Gastric Cancer Screening**
One prominent advantage of sleeve-plus procedures is their suitability for screening the remaining stomach for gastric cancer. This is particularly important in regions with a high prevalence of gastric cancer, such as Japan and Korea [23]. In contrast, performing this screening in the case of Roux-en-Y Gastric Bypass (RYGB) can be challenging.
**2. Preservation of the Pylorus**
In techniques where anatomical and functional preservation of the pylorus is a priority, sleeve-plus procedures stand out. This preservation shields the gastric mucosa from the potentially harmful effects of pancreatic and biliary fluids, effectively preventing bile acid gastritis [24]. Additionally, the pylorus plays a crucial role in regulating gastric emptying, resulting in a lower incidence of dumping syndrome [25]. The increased contact of gastric mucosa with food in Sleeve Gastrectomy (SG) compared to RYGB enhances the absorption of essential nutrients like iron, calcium, vitamin B12, and protein, thereby reducing the risk of nutritional deficiencies [26].
**3. Conversion Flexibility**
Sleeve-plus procedures exhibit remarkable versatility when it comes to conversions to other surgical options. Whether it's due to weight regain or complications like leaks and strictures, the ability to convert to alternative procedures is a valuable feature. For example, the loop SGDJB can be transformed into a Duodenal Switch (DS) by modifying the afferent limb and anastomosing it to the distal segment of the efferent limb. The Roux-en-Y SGDJB is also convertible to DS by extending the alimentary limb from the biliopancreatic limb. Even conversion to RYGB from any sleeve-plus procedure is a feasible option. In cases of sleeve-plus procedures with a transected duodenum, the proximal duodenal anastomosis must be dismantled, allowing for the resection of the distal gastric tube. The previous alimentary limb is then anastomosed to the remaining gastric pouch. In an SGPJB, a gastric pouch is simply created and anastomosed to the blind limb, constructing the alimentary limb. In SG with bipartition, the gastroenteric anastomosis is transected, followed by creating a gastric pouch and performing a Roux-en-Y reconstruction of the bowel.
**4. Loop Techniques: Efficiency and Reduced Complications**
Loop techniques within sleeve-plus procedures offer an additional advantage over Roux-en-Y techniques. The presence of a single anastomosis in loop procedures results in a shorter operative time and a decreased potential for complications that may arise from multiple anastomoses. Furthermore, loop techniques have not been associated with marginal ulcers [20], which may be attributed to the prompt neutralization of gastric fluid by bile juices once they reach the duodenum.
In summary, sleeve-plus procedures bring a multitude of benefits to the table, from facilitating gastric cancer screening and preserving the pylorus to offering conversion flexibility and reducing the risk of complications. These advantages make sleeve-plus procedures a promising option for individuals seeking effective and sustainable weight loss with the added benefit of improved health outcomes.
sleeve gastrectomy with bypass, sleeve-plus, duodenojejunal bypass, proximal jejunal bypass, morbid obesity, type 2 diabetes, bariatric surgery in Asia
Obesity is a global epidemic, with an increasing number of bariatric surgeries being performed to combat it. While Roux-en-Y gastric bypass (RYGB) has long been considered the gold standard for bariatric surgery due to its effectiveness in weight loss and remission of type 2 Diabetes Mellitus (T2DM), the technical complexity and postoperative complications have led to a rise in the popularity of sleeve gastrectomy (SG). However, SG has its own limitations, such as long-term weight regain and the recurrence of co-morbidities.
In an effort to improve outcomes and reduce complications, new procedures have emerged, particularly the addition of an intestinal bypass to SG, resulting in what is termed "sleeve-plus" procedures. This chapter will provide an in-depth discussion of sleeve-plus techniques commonly performed in the Asia-Pacific region, specifically the duodenojejunal bypass (DJB) and the proximal jejunal bypass (PJB).
World Statistics and Census
Obesity is a major non-communicable epidemic disease that has been on the rise worldwide. The International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) reports a significant number of bariatric surgeries, with SG and RYGB being the most common procedures. In the Asia-Pacific region, countries like Australia and the Gulf have reported a high number of surgeries, mainly SG. RYGB remains the gold standard, but due to its technical challenges and complications, SG has gained popularity.
Brief Evolution of Bariatric Surgery
Bariatric and metabolic surgery has evolved significantly since its early days. The first procedures, such as the jejunoileal bypass and gastric bypass, were developed in the mid-20th century, with varying degrees of success and complications. SG emerged as a standalone procedure and became a popular choice due to its effectiveness.
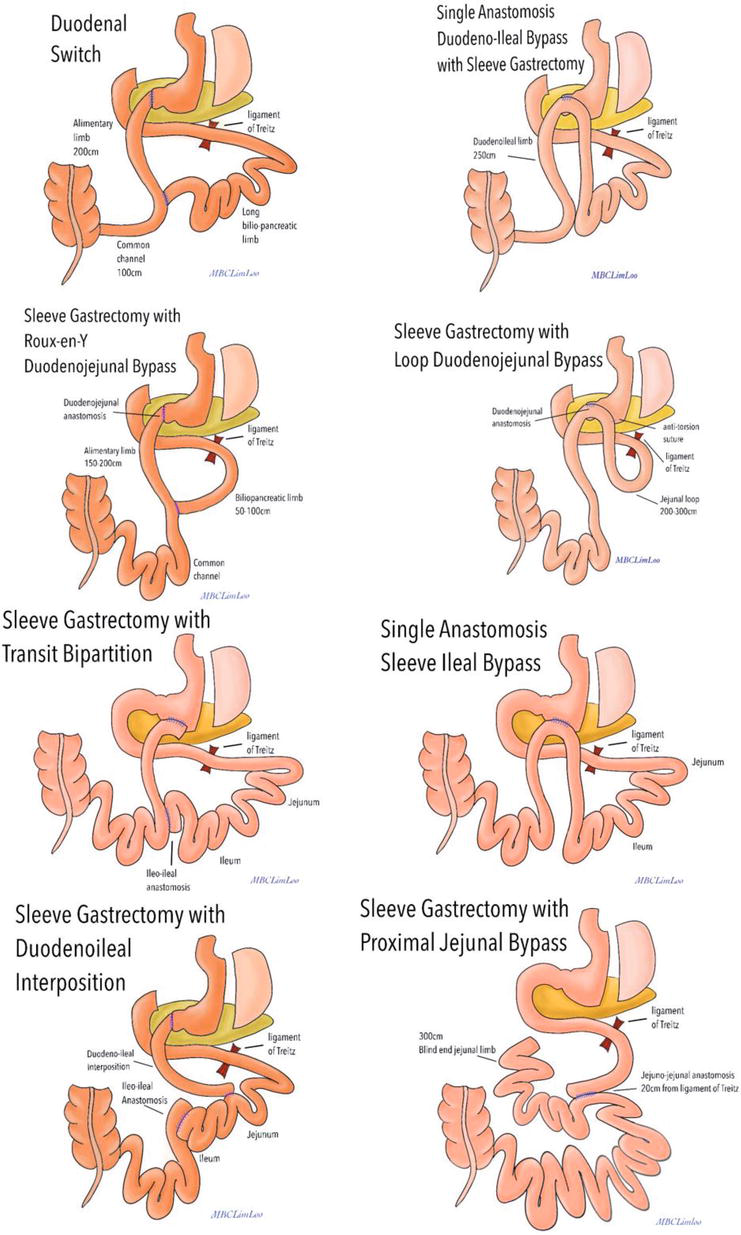
Types of Sleeve-Plus Procedures
Several sleeve-plus procedures have been developed, each with its unique characteristics. These include BPDDS, SADI-S, SASI, SGDJB, IISG, and SGPJB. These procedures vary in terms of anatomical alterations, limb reconstruction, and the location of limb anastomosis.
Advantages of Sleeve-Plus Procedures
Sleeve-plus procedures offer various advantages. They allow for the screening of the remaining stomach for gastric cancer, making them particularly valuable in regions with a high prevalence of gastric cancer. Additionally, procedures that preserve the pylorus protect the gastric mucosa from harmful fluids and help regulate gastric emptying, reducing the risk of dumping syndrome. The increased contact of gastric mucosa with food in SG compared to RYGB also enhances nutrient absorption, reducing nutritional deficiencies. Furthermore, these procedures are versatile and can be converted to other bariatric surgeries if necessary.
Hormonal Effect of Sleeve-Plus Procedures
Sleeve-plus procedures affect the entero-insular axis, influencing gastrointestinal, endocrine, and pancreatic secretions involved in insulin production. These procedures have a positive impact on glucose homeostasis, with the "foregut" and "hindgut" theories explaining their mechanisms. Hormonal changes such as decreased ghrelin levels and increased GLP-1 and PYY levels play a crucial role in improved glycemic control.
Indications and Contraindications
Indications for bariatric surgery have evolved over time and vary by region. Factors such as BMI and the presence of co-morbidities are considered when determining eligibility. Contraindications include physiological, medical, surgical, and psychological factors. Smoking and poorly controlled eating disorders are among the relative contraindications.
Selection of Sleeve-Plus Procedure
The choice between different sleeve-plus procedures depends on various factors, including BMI, diabetes history, surgical findings, and the patient's medical condition. Considerations for safety and optimal outcomes are paramount.
Preoperative Considerations
A comprehensive preoperative evaluation is crucial, involving a multidisciplinary team that assesses medical and psychological factors. A thorough medical history, physical examination, and preoperative work-up are conducted to ensure that the patient is well-prepared for the procedure.
In conclusion, sleeve-plus procedures offer promising options for the treatment of obesity and T2DM. These innovative techniques combine the advantages of SG with the physiological changes seen in RYGB, while minimizing adverse effects. The choice of procedure should be based on individual patient characteristics and considerations for safety and efficacy. A holistic approach to preoperative evaluation and patient education is key to achieving successful outcomes in bariatric surgery.
| Older Post | Home | Newer Post |

