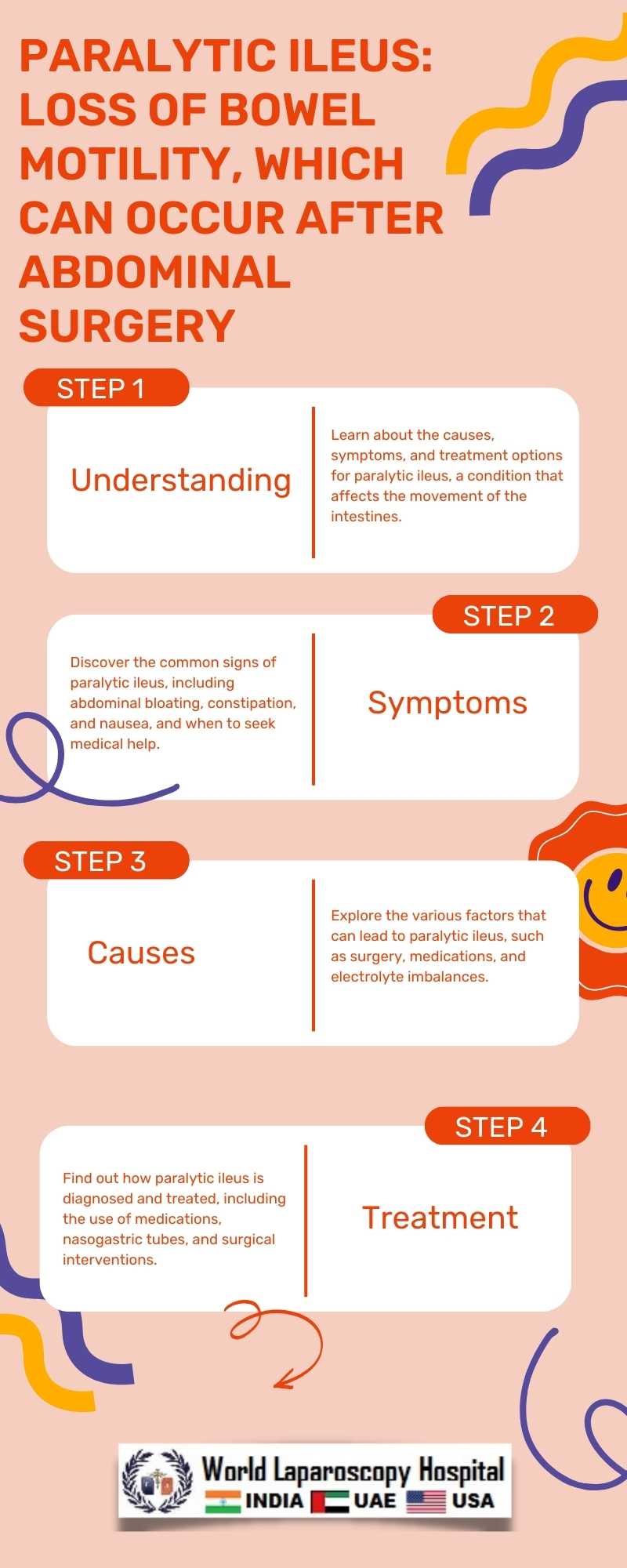
Paralytic ileus: Loss of bowel motility, which can occur after abdominal surgery
Paralytic ileus is a condition characterized by the temporary loss of normal bowel movement (peristalsis). It is a common complication that can occur after abdominal surgery, leading to significant morbidity and prolonging hospital stays. Understanding the causes, symptoms, diagnosis, and management of paralytic ileus is crucial for healthcare providers to effectively manage this condition and improve patient outcomes.
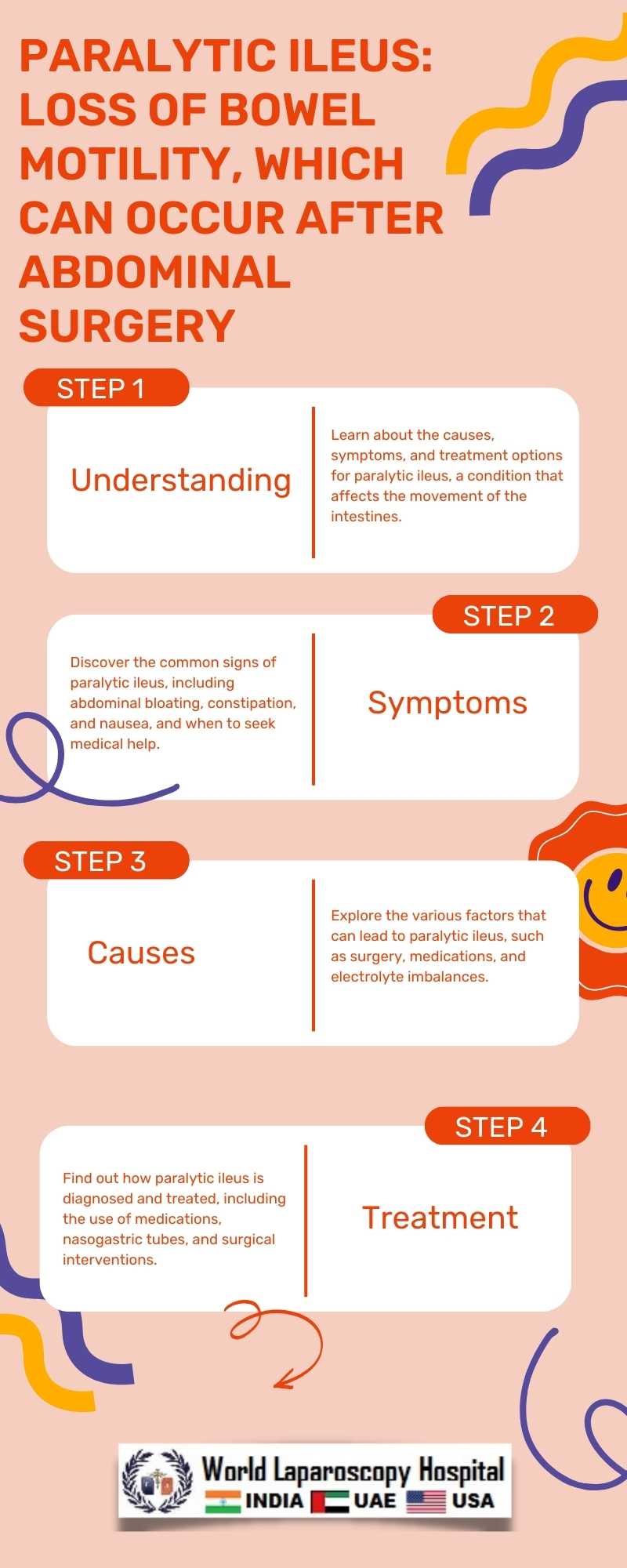
One of the primary causes of paralytic ileus after abdominal surgery is the manipulation of the intestines during the procedure. Surgical trauma, handling of the intestines, and the use of anesthesia can lead to a temporary disruption of the normal rhythmic contractions of the intestines. This disruption can result in the accumulation of gas and fluids, leading to bloating, distension, and discomfort.
Symptoms of paralytic ileus can vary from mild to severe and may include abdominal distension, lack of bowel movements, nausea, vomiting, and a decrease in bowel sounds. Patients may also experience pain and discomfort in the abdomen. These symptoms can develop within a few hours to a few days after surgery and can significantly impact the patient's recovery and quality of life.
Diagnosing paralytic ileus involves a thorough medical history, physical examination, and imaging studies such as X-rays or CT scans. The absence of bowel sounds and the presence of abdominal distension are key findings in the diagnosis of paralytic ileus. Laboratory tests may also be performed to rule out other possible causes of the symptoms.
Management of paralytic ileus focuses on supportive care and measures to stimulate bowel function. Patients are typically kept NPO (nothing by mouth) to rest the bowel and prevent further stimulation. Intravenous fluids are administered to maintain hydration, and nasogastric suction may be used to decompress the stomach and intestines. Early ambulation and the use of medications such as prokinetic agents may help stimulate bowel motility and shorten the duration of ileus.
In severe cases, surgical intervention may be required to relieve obstruction or remove any adhesions that may be causing the ileus. However, most cases of paralytic ileus resolve with conservative management within a few days to a week. Close monitoring of the patient's condition is essential to prevent complications such as bowel perforation or ischemia.
Conclusion:
Paralytic ileus is a common complication that can occur after abdominal surgery. Understanding the causes, symptoms, diagnosis, and management of this condition is essential for healthcare providers to provide appropriate care and improve patient outcomes. Early recognition and prompt intervention can help minimize the impact of paralytic ileus on patient recovery and quality of life.
One of the primary causes of paralytic ileus after abdominal surgery is the manipulation of the intestines during the procedure. Surgical trauma, handling of the intestines, and the use of anesthesia can lead to a temporary disruption of the normal rhythmic contractions of the intestines. This disruption can result in the accumulation of gas and fluids, leading to bloating, distension, and discomfort.
Symptoms of paralytic ileus can vary from mild to severe and may include abdominal distension, lack of bowel movements, nausea, vomiting, and a decrease in bowel sounds. Patients may also experience pain and discomfort in the abdomen. These symptoms can develop within a few hours to a few days after surgery and can significantly impact the patient's recovery and quality of life.
Diagnosing paralytic ileus involves a thorough medical history, physical examination, and imaging studies such as X-rays or CT scans. The absence of bowel sounds and the presence of abdominal distension are key findings in the diagnosis of paralytic ileus. Laboratory tests may also be performed to rule out other possible causes of the symptoms.
Management of paralytic ileus focuses on supportive care and measures to stimulate bowel function. Patients are typically kept NPO (nothing by mouth) to rest the bowel and prevent further stimulation. Intravenous fluids are administered to maintain hydration, and nasogastric suction may be used to decompress the stomach and intestines. Early ambulation and the use of medications such as prokinetic agents may help stimulate bowel motility and shorten the duration of ileus.
In severe cases, surgical intervention may be required to relieve obstruction or remove any adhesions that may be causing the ileus. However, most cases of paralytic ileus resolve with conservative management within a few days to a week. Close monitoring of the patient's condition is essential to prevent complications such as bowel perforation or ischemia.
Conclusion:
Paralytic ileus is a common complication that can occur after abdominal surgery. Understanding the causes, symptoms, diagnosis, and management of this condition is essential for healthcare providers to provide appropriate care and improve patient outcomes. Early recognition and prompt intervention can help minimize the impact of paralytic ileus on patient recovery and quality of life.
2 COMMENTS
Dr. Kriti
#1
Feb 26th, 2024 5:48 am
Paralytic ileus post-abdominal surgery demands comprehensive understanding from healthcare providers. Recognizing causes, symptoms, diagnosis, and management is crucial for optimal care and patient outcomes. Early identification and intervention mitigate its impact on recovery and quality of life.
Dr. Aditi Shruti
#2
Feb 27th, 2024 4:36 pm
Paralytic ileus post-abdominal surgery warrants comprehensive understanding by healthcare providers. Early recognition and intervention are pivotal in mitigating its impact on patient recovery and quality of life. Expert management ensures optimal care and improved outcomes.
| Older Post | Home | Newer Post |

