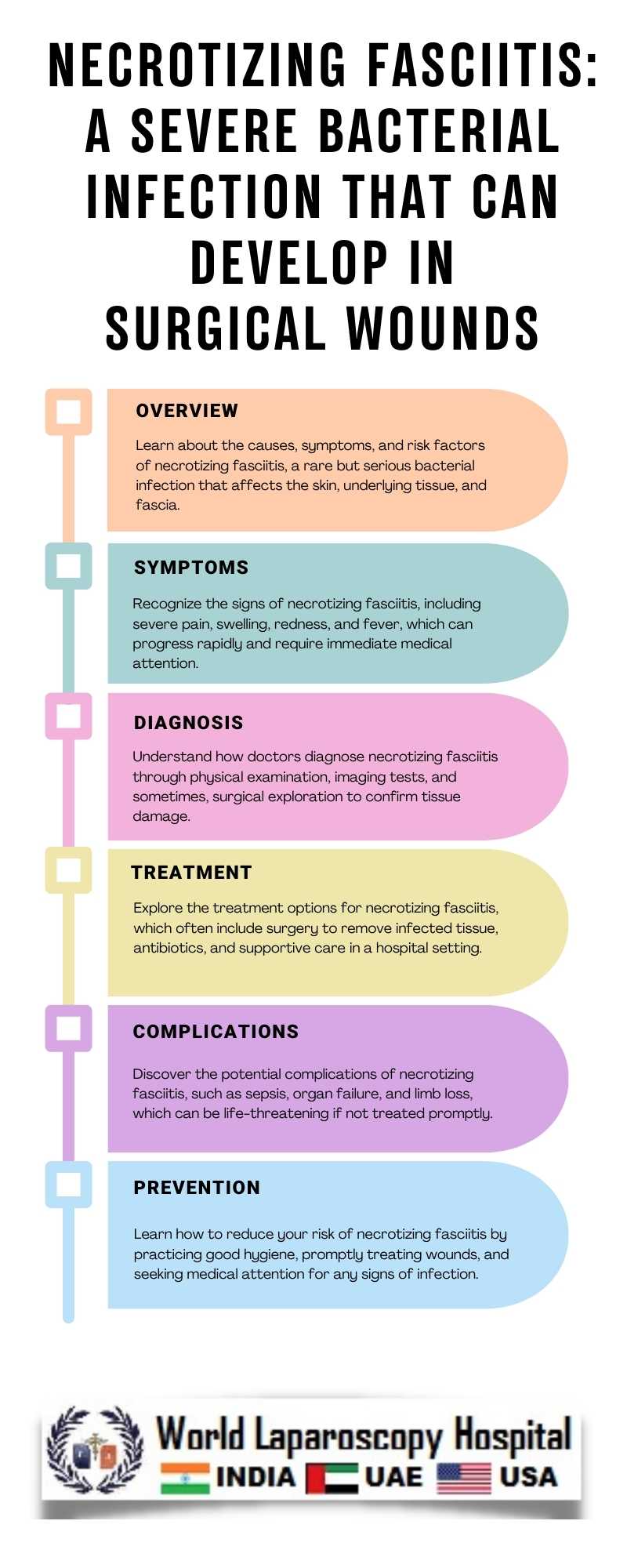
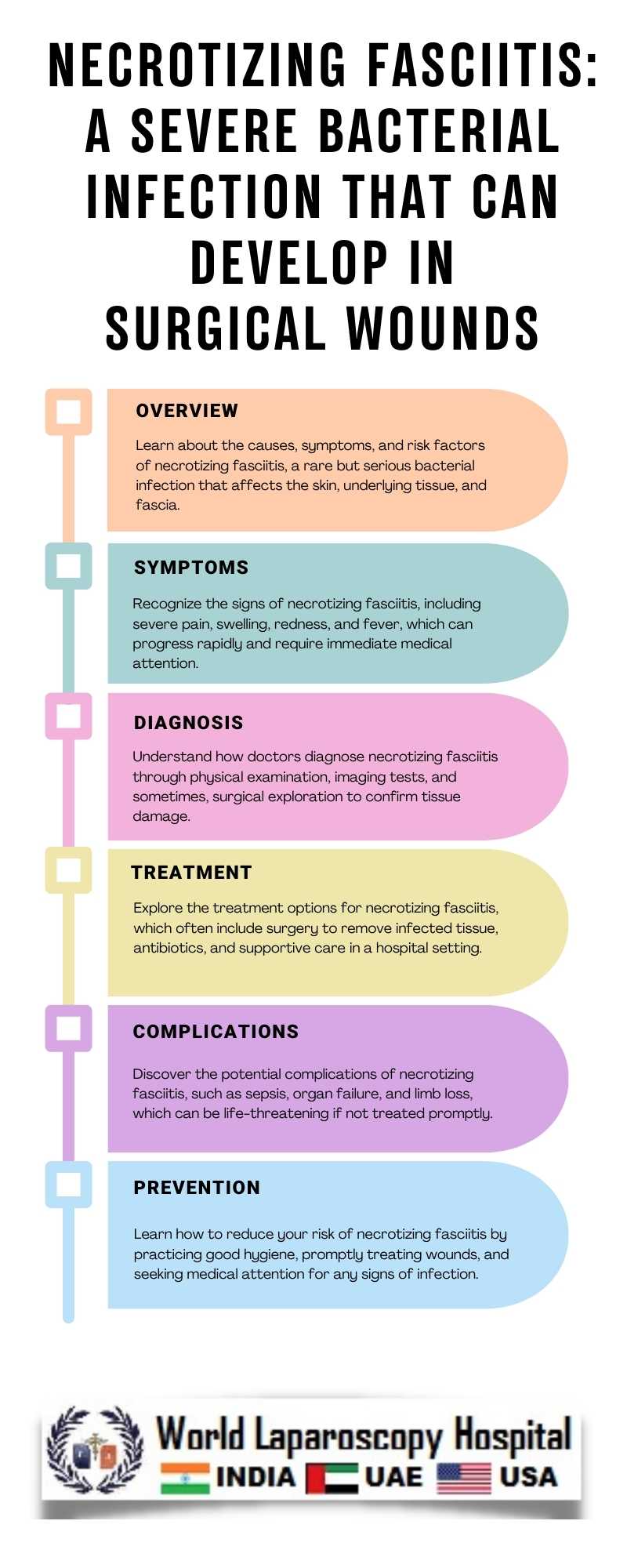
Necrotizing fasciitis: A severe bacterial infection that can develop in surgical wounds
Necrotizing Fasciitis: A Silent Threat in Surgical Recovery
Surgery, a beacon of hope for many battling illness or injury, can sometimes bring unexpected challenges. One such challenge is necrotizing fasciitis, a rare but potentially life-threatening bacterial infection that can develop in surgical wounds. This condition, often referred to as "flesh-eating bacteria," demands swift recognition and aggressive treatment to prevent devastating consequences.
Understanding Necrotizing Fasciitis
Necrotizing fasciitis is a severe infection that targets the body's soft tissues, particularly the fascia, a layer of tissue beneath the skin that surrounds muscles, nerves, and blood vessels. The infection rapidly destroys this tissue, leading to necrosis (death of the tissue) and can progress to affect surrounding organs and systems if not promptly treated.
Causes and Risk Factors
The infection is typically caused by a group of bacteria, including Streptococcus and Staphylococcus, which enter the body through a break in the skin, such as a surgical incision. Certain factors can increase the risk of developing necrotizing fasciitis, including:
- Chronic health conditions like diabetes, which can weaken the immune system
- Obesity, which can impair blood flow and increase the likelihood of tissue damage
- Recent surgery or trauma, providing an entry point for bacteria
- Immunosuppressive medications, which can reduce the body's ability to fight infections
Recognizing the Symptoms
Early recognition of necrotizing fasciitis is crucial for successful treatment. Symptoms can vary but may include:
- Severe pain that is disproportionate to the visible wound
- Swelling, redness, or warmth around the wound site
- Fever, chills, and overall malaise
- Rapid progression of symptoms, with the condition worsening quickly
Treatment and Management
Immediate medical attention is essential if necrotizing fasciitis is suspected. Treatment typically involves a combination of surgical intervention and antibiotic therapy. Surgery is aimed at removing the infected tissue to prevent the further spread of the infection. Antibiotics are administered to help fight the bacteria causing the infection.
Prevention Strategies
While necrotizing fasciitis is rare, there are steps that can be taken to reduce the risk, especially in surgical settings. These include:
- Strict adherence to infection control practices before, during, and after surgery
- Thorough cleaning and sterilization of surgical instruments
- Monitoring and promptly treating any signs of infection in surgical wounds
- Educating patients on proper wound care post-surgery
Conclusion
Necrotizing fasciitis, though rare, is a serious complication that can occur after surgery. Vigilance and prompt action are key to managing this condition effectively. By understanding the risk factors, recognizing the symptoms, and implementing preventive measures, healthcare providers can help minimize the impact of this potentially devastating infection on their patients' lives.
Surgery, a beacon of hope for many battling illness or injury, can sometimes bring unexpected challenges. One such challenge is necrotizing fasciitis, a rare but potentially life-threatening bacterial infection that can develop in surgical wounds. This condition, often referred to as "flesh-eating bacteria," demands swift recognition and aggressive treatment to prevent devastating consequences.
Understanding Necrotizing Fasciitis
Necrotizing fasciitis is a severe infection that targets the body's soft tissues, particularly the fascia, a layer of tissue beneath the skin that surrounds muscles, nerves, and blood vessels. The infection rapidly destroys this tissue, leading to necrosis (death of the tissue) and can progress to affect surrounding organs and systems if not promptly treated.
Causes and Risk Factors
The infection is typically caused by a group of bacteria, including Streptococcus and Staphylococcus, which enter the body through a break in the skin, such as a surgical incision. Certain factors can increase the risk of developing necrotizing fasciitis, including:
- Chronic health conditions like diabetes, which can weaken the immune system
- Obesity, which can impair blood flow and increase the likelihood of tissue damage
- Recent surgery or trauma, providing an entry point for bacteria
- Immunosuppressive medications, which can reduce the body's ability to fight infections
Recognizing the Symptoms
Early recognition of necrotizing fasciitis is crucial for successful treatment. Symptoms can vary but may include:
- Severe pain that is disproportionate to the visible wound
- Swelling, redness, or warmth around the wound site
- Fever, chills, and overall malaise
- Rapid progression of symptoms, with the condition worsening quickly
Treatment and Management
Immediate medical attention is essential if necrotizing fasciitis is suspected. Treatment typically involves a combination of surgical intervention and antibiotic therapy. Surgery is aimed at removing the infected tissue to prevent the further spread of the infection. Antibiotics are administered to help fight the bacteria causing the infection.
Prevention Strategies
While necrotizing fasciitis is rare, there are steps that can be taken to reduce the risk, especially in surgical settings. These include:
- Strict adherence to infection control practices before, during, and after surgery
- Thorough cleaning and sterilization of surgical instruments
- Monitoring and promptly treating any signs of infection in surgical wounds
- Educating patients on proper wound care post-surgery
Conclusion
Necrotizing fasciitis, though rare, is a serious complication that can occur after surgery. Vigilance and prompt action are key to managing this condition effectively. By understanding the risk factors, recognizing the symptoms, and implementing preventive measures, healthcare providers can help minimize the impact of this potentially devastating infection on their patients' lives.
2 COMMENTS
Dr. Ekta Keshwani
#1
Feb 24th, 2024 6:55 am
Necrotizing fasciitis, albeit uncommon, poses a severe post-surgery threat. Timely vigilance and intervention are paramount. Healthcare providers must comprehend risk factors, identify symptoms, and enact preventive strategies to mitigate the potential devastation of this infection.
Dr. Zenna Burgos
#2
Feb 26th, 2024 10:01 am
Necrotizing fasciitis, although uncommon post-surgery, demands vigilant monitoring and swift intervention. Understanding risk factors, symptoms, and preventive measures empowers healthcare providers to mitigate its potentially devastating impact on patients' lives effectively.
| Older Post | Home | Newer Post |


