Postoperative peritonitis: Inflammation of the peritoneum, often due to infection after abdominal surgery
Introduction
Postoperative peritonitis is a serious complication that can occur after abdominal surgery, characterized by inflammation of the peritoneum, the membrane lining the abdominal cavity. This condition can be caused by various factors, most commonly by a bacterial infection that enters the peritoneal cavity during or after surgery. Understanding the causes, symptoms, diagnosis, and management of postoperative peritonitis is crucial for surgeons and healthcare providers to ensure timely intervention and improved patient outcomes.
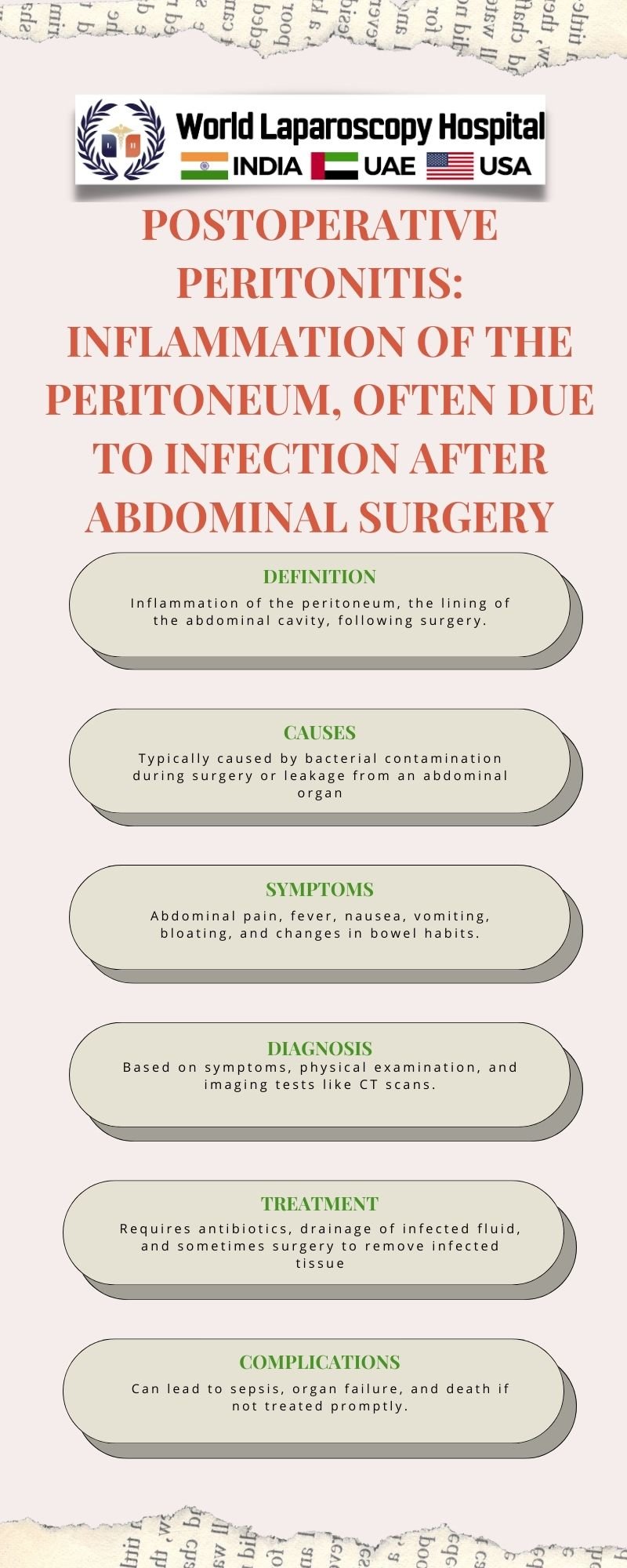
Causes of Postoperative Peritonitis Postoperative peritonitis can result from several factors, including:
Perforation of the gastrointestinal tract:
During abdominal surgery, accidental perforation of the stomach, intestines, or other organs can occur, allowing the contents of the gastrointestinal tract to leak into the peritoneal cavity. This can lead to a severe inflammatory response and infection.
Contamination during surgery:
Despite strict sterile techniques, surgical procedures can sometimes lead to contamination of the peritoneal cavity with bacteria from the skin, instruments, or other sources.
Anastomotic leaks:
In procedures involving the creation of anastomoses (connections) between different parts of the gastrointestinal tract, leaks can occur at the site of the anastomosis, leading to peritoneal contamination.
Ischemic bowel:
Inadequate blood supply to a segment of the bowel during surgery can result in ischemia (lack of oxygen), leading to tissue damage and subsequent infection.
Foreign body reaction:
Sometimes, the presence of foreign bodies, such as surgical meshes or sutures, can trigger an inflammatory response in the peritoneum, leading to peritonitis.
Symptoms of Postoperative Peritonitis The symptoms of postoperative peritonitis can vary depending on the severity of the condition and the underlying cause. However, common symptoms may include:
- Severe abdominal pain that may be localized or diffuse
- Abdominal tenderness and rigidity
- Fever and chills
- Nausea and vomiting
- Distension of the abdomen
- Absent or decreased bowel sounds
- Signs of systemic infection, such as tachycardia (rapid heart rate) and tachypnea (rapid breathing)
Diagnosis of Postoperative Peritonitis Diagnosing postoperative peritonitis requires a thorough evaluation of the patient's clinical history, physical examination, and laboratory and imaging studies. Key steps in the diagnostic process include:
Clinical assessment:
The surgeon assesses the patient's symptoms, including the nature and duration of abdominal pain, presence of fever, and other signs of peritonitis.
Laboratory tests:
Blood tests, including a complete blood count (CBC) and inflammatory markers such as C-reactive protein (CRP) and procalcitonin, can help assess the severity of the inflammatory response and presence of infection.
Imaging studies:
Imaging tests such as abdominal ultrasound, CT scan, or MRI may be performed to identify the underlying cause of peritonitis, such as perforation, abscess formation, or anastomotic leak.
Diagnostic peritoneal lavage (DPL):
In some cases, a DPL may be performed to obtain peritoneal fluid for analysis, which can help confirm the diagnosis of peritonitis and identify the causative organism.
Management of Postoperative Peritonitis The management of postoperative peritonitis involves a combination of supportive care, antibiotic therapy, and surgical intervention. The goals of treatment are to control the infection, remove the source of contamination, and prevent further complications. Key aspects of management include:
Supportive care:
Patients with postoperative peritonitis may require fluid resuscitation, electrolyte replacement, and nutritional support to maintain adequate hydration and nutrition.
Antibiotic therapy:
Empirical antibiotic therapy is initiated based on the likely causative organisms and adjusted according to culture and sensitivity results. Broad-spectrum antibiotics are often used initially to cover a wide range of potential pathogens.
Surgical intervention:
In cases where there is a clear source of contamination, such as a perforated viscus or anastomotic leak, surgical intervention is necessary to repair the defect and drain any abscesses that may have formed.
Source control:
Source control measures, such as drainage of infected fluid collections and removal of necrotic tissue, are essential to eliminate the source of infection and prevent recurrence.
Monitoring and follow-up:
Patients with postoperative peritonitis require close monitoring of their clinical status, laboratory parameters, and imaging studies to assess the response to treatment and detect any complications early.
Conclusion
Postoperative peritonitis is a serious complication of abdominal surgery that requires prompt recognition and intervention to improve patient outcomes. Surgeons and healthcare providers should be aware of the causes, symptoms, diagnosis, and management of this condition to provide timely and effective care to affected patients. Collaborative efforts between surgical teams, infectious disease specialists, and critical care teams are essential for the optimal management of postoperative peritonitis and the prevention of complications.
| Older Post | Home | Newer Post |


