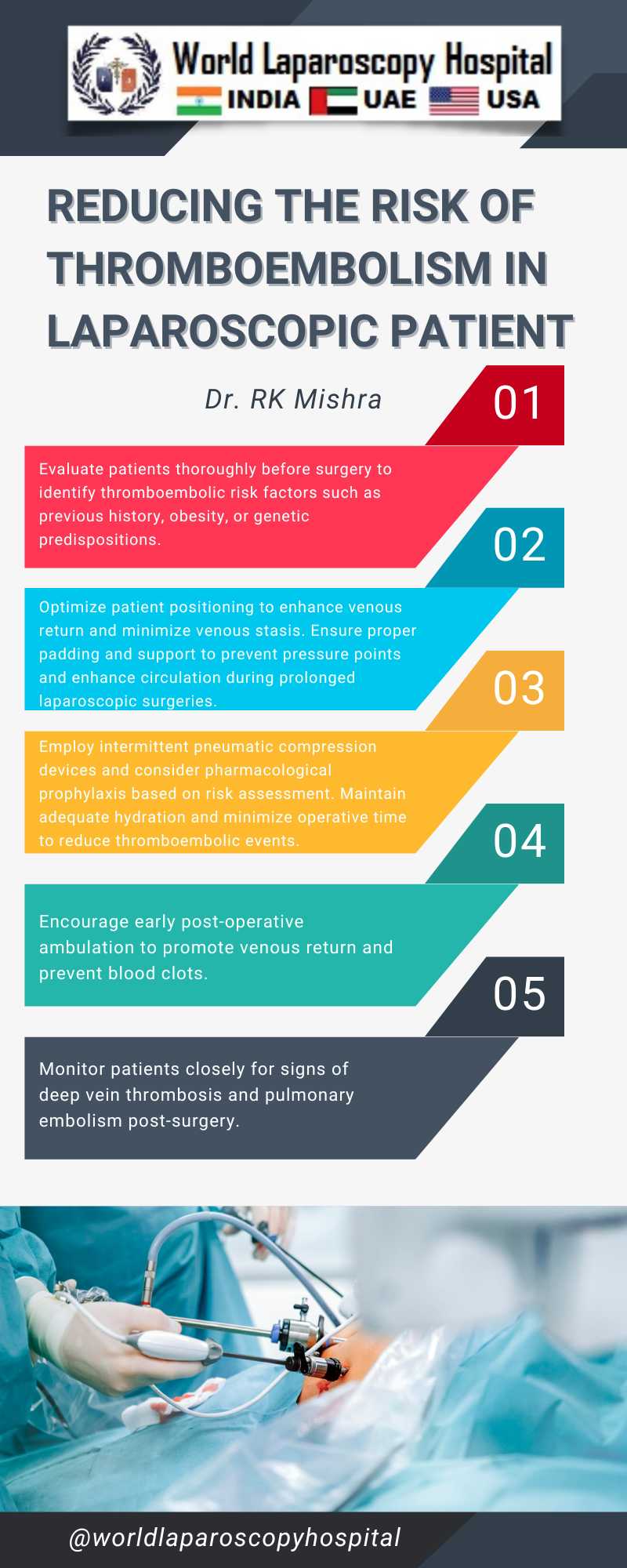
Reducing the Risk of Thromboembolism in Laparoscopic Patient
Reducing the risk of thromboembolism in patients undergoing laparoscopic surgery is a crucial aspect of perioperative care, given the unique challenges posed by the minimally invasive nature of these procedures. Thromboembolism, which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), represents a significant risk due to factors such as patient immobility, the use of pneumoperitoneum, and the positioning of the patient during surgery. This essay outlines strategies to mitigate these risks, focusing on patient assessment, pharmacological prophylaxis, mechanical interventions, and intraoperative considerations.
Patient Assessment and Risk Stratification
Prior to surgery, a thorough assessment of the patient's risk for thromboembolism is essential. This involves evaluating individual risk factors such as age, history of thromboembolism, obesity, malignancy, hormonal therapy, and genetic predispositions. Tools like the Caprini Risk Assessment Model can help in stratifying patients into different risk categories, guiding the selection of appropriate prophylactic measures.
Pharmacological Prophylaxis
Anticoagulant therapy plays a pivotal role in preventing DVT and PE in high-risk patients. The choice of agent (e.g., low molecular weight heparins, unfractionated heparin, or oral anticoagulants) and the duration of therapy depend on the patient's risk profile and the nature of the surgical procedure. It is crucial to balance the benefits of thromboprophylaxis with the risk of bleeding, particularly in the context of minimally invasive surgery where surgical field visibility is paramount.
Mechanical Interventions
Mechanical methods, such as graduated compression stockings (GCS) and intermittent pneumatic compression (IPC) devices, are effective in enhancing venous blood flow and reducing stasis, a key component in the pathogenesis of DVT. These non-invasive measures are particularly useful in patients where pharmacological prophylaxis is contraindicated. Ensuring proper application and usage of these devices is vital for their effectiveness.
Intraoperative Considerations
The laparoscopic approach inherently carries specific risks related to thromboembolism. The creation of pneumoperitoneum increases intra-abdominal pressure, which can reduce venous return and enhance venous stasis. Moreover, patient positioning, such as the Trendelenburg position, may further exacerbate these effects. To mitigate these risks, it is advisable to minimize the duration of surgery, optimize the intra-abdominal pressure to the lowest effective level, and encourage early mobilization postoperatively. Additionally, the use of intraoperative mechanical prophylaxis, such as IPC devices, can be beneficial.
Postoperative Care and Early Mobilization
Early mobilization following surgery is a key strategy in reducing the risk of thromboembolic events. Encouraging patients to ambulate as soon as safely possible after surgery can significantly decrease the incidence of DVT. This, combined with continued use of pharmacological and mechanical prophylaxis as indicated, forms an integral part of the postoperative care plan.
Conclusion
The prevention of thromboembolism in patients undergoing laparoscopic surgery requires a multifaceted approach that includes thorough risk assessment, judicious use of pharmacological agents, application of mechanical prophylactic measures, and attention to intraoperative and postoperative care practices. Tailoring these strategies to individual patient risk profiles and the specifics of the surgical procedure is paramount in minimizing the risk of these potentially life-threatening complications.
Patient Assessment and Risk Stratification
Prior to surgery, a thorough assessment of the patient's risk for thromboembolism is essential. This involves evaluating individual risk factors such as age, history of thromboembolism, obesity, malignancy, hormonal therapy, and genetic predispositions. Tools like the Caprini Risk Assessment Model can help in stratifying patients into different risk categories, guiding the selection of appropriate prophylactic measures.
Pharmacological Prophylaxis
Anticoagulant therapy plays a pivotal role in preventing DVT and PE in high-risk patients. The choice of agent (e.g., low molecular weight heparins, unfractionated heparin, or oral anticoagulants) and the duration of therapy depend on the patient's risk profile and the nature of the surgical procedure. It is crucial to balance the benefits of thromboprophylaxis with the risk of bleeding, particularly in the context of minimally invasive surgery where surgical field visibility is paramount.
Mechanical Interventions
Mechanical methods, such as graduated compression stockings (GCS) and intermittent pneumatic compression (IPC) devices, are effective in enhancing venous blood flow and reducing stasis, a key component in the pathogenesis of DVT. These non-invasive measures are particularly useful in patients where pharmacological prophylaxis is contraindicated. Ensuring proper application and usage of these devices is vital for their effectiveness.
Intraoperative Considerations
The laparoscopic approach inherently carries specific risks related to thromboembolism. The creation of pneumoperitoneum increases intra-abdominal pressure, which can reduce venous return and enhance venous stasis. Moreover, patient positioning, such as the Trendelenburg position, may further exacerbate these effects. To mitigate these risks, it is advisable to minimize the duration of surgery, optimize the intra-abdominal pressure to the lowest effective level, and encourage early mobilization postoperatively. Additionally, the use of intraoperative mechanical prophylaxis, such as IPC devices, can be beneficial.
Postoperative Care and Early Mobilization
Early mobilization following surgery is a key strategy in reducing the risk of thromboembolic events. Encouraging patients to ambulate as soon as safely possible after surgery can significantly decrease the incidence of DVT. This, combined with continued use of pharmacological and mechanical prophylaxis as indicated, forms an integral part of the postoperative care plan.
Conclusion
The prevention of thromboembolism in patients undergoing laparoscopic surgery requires a multifaceted approach that includes thorough risk assessment, judicious use of pharmacological agents, application of mechanical prophylactic measures, and attention to intraoperative and postoperative care practices. Tailoring these strategies to individual patient risk profiles and the specifics of the surgical procedure is paramount in minimizing the risk of these potentially life-threatening complications.
1 COMMENTS
Dr. Mugdha Khatri
#1
Jan 27th, 2024 8:51 am
Mitigating thromboembolism risk in laparoscopic surgery demands meticulous perioperative care. This essay meticulously explores strategies, emphasizing patient assessment, pharmacological prophylaxis, mechanical interventions, and intraoperative considerations to counteract unique challenges posed by minimally invasive procedures.
| Older Post | Home | Newer Post |





