Techniques and Tips to Prevent Gas Embolism During Laparoscopic Procedures
Introduction:
Laparoscopic surgery has revolutionized the field of minimally invasive procedures, offering numerous benefits such as quicker recovery times, reduced postoperative pain, and smaller incisions. However, like any medical intervention, it comes with its own set of risks, and one of the potentially life-threatening complications is gas embolism. Gas embolism occurs when gas bubbles enter the bloodstream, obstructing blood vessels and potentially leading to severe consequences. In laparoscopic surgeries, where carbon dioxide is commonly used to create a working space, preventing gas embolism is crucial. This article explores advanced techniques and essential tips to enhance safety and prevent gas embolism during laparoscopic procedures.
Understanding Gas Embolism:
Gas embolism during laparoscopic surgery can arise from several sources, such as insufflation of gas, accidental vessel injury, or gas leakage. The consequences range from mild symptoms to fatal outcomes, emphasizing the need for proactive prevention strategies.
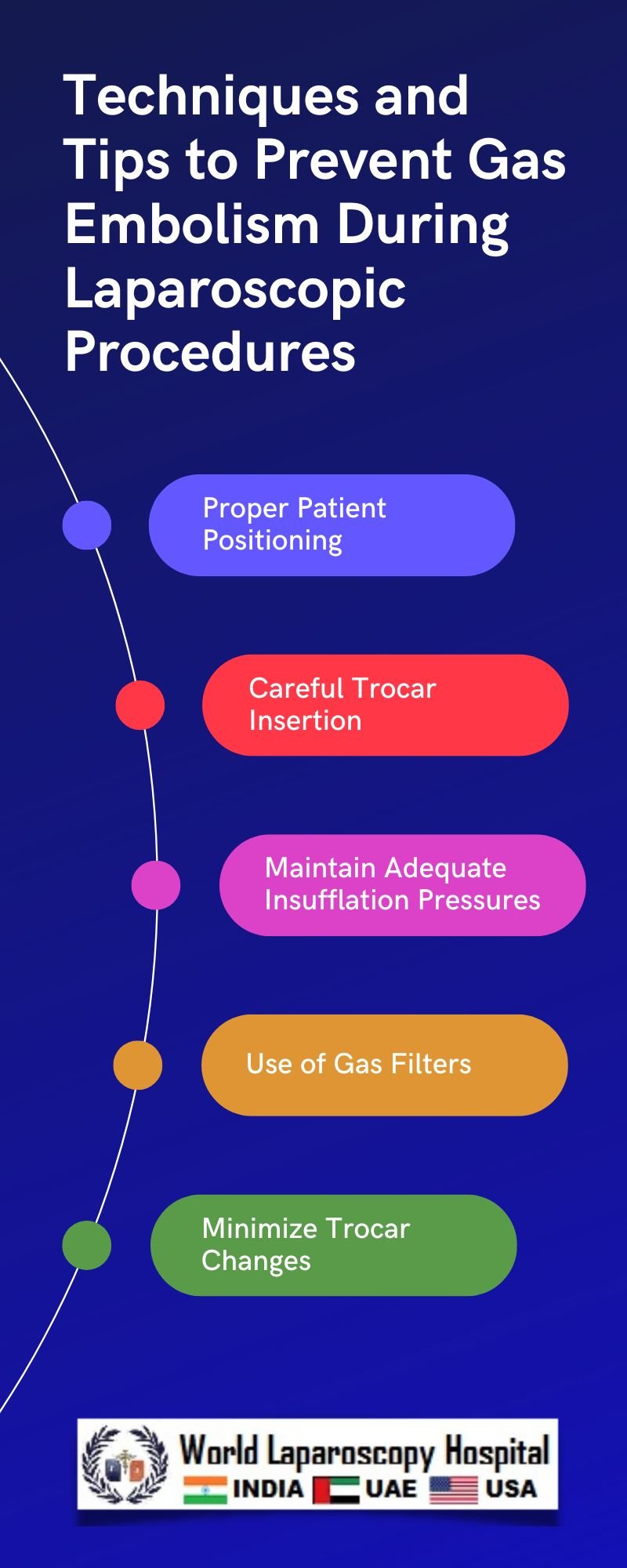
Precise Insufflation Techniques:Proper insufflation is paramount in laparoscopic procedures. Surgeons must use precise insufflation pressures and flow rates to create and maintain the pneumoperitoneum. High pressures and rapid insufflation can lead to barotrauma, causing vascular injury and gas embolism. Utilizing pressure monitoring devices and slow insufflation techniques can significantly reduce the risk.
Gas Quality and Humidification:The quality of insufflated gas plays a crucial role in preventing complications. Dry and cold carbon dioxide can cause endothelial damage, potentially leading to gas embolism. Surgeons should consider using humidified and warmed gas to minimize the risk of vascular injury.
Optimal Trocar Placement:Careful trocar placement is essential to prevent inadvertent vessel injury during laparoscopic entry. Surgeons should avoid blind trocar insertion and use visual confirmation methods, such as direct visualization or ultrasound guidance, to ensure trocars are safely placed, minimizing the risk of gas embolism.
Gas Leak Prevention:Preventing gas leaks is a fundamental aspect of avoiding gas embolism. Regular equipment maintenance, checking for potential leaks, and using high-quality trocars and cannulas contribute to a secure operative environment. Surgeons should be vigilant for any signs of gas leakage and address them promptly.
Monitoring and Immediate Recognition:Continuous monitoring of patient parameters, such as end-tidal CO2 levels, central venous pressure, and oxygen saturation, is crucial for early detection of gas embolism. Rapid recognition allows for immediate intervention, such as changing patient positioning, adjusting insufflation pressures, or converting to an open procedure if necessary.
Trendelenburg Positioning:In the event of suspected gas embolism, placing the patient in the Trendelenburg position (head down) can help trap gas in the right atrium, preventing it from traveling to the cerebral circulation. This maneuver can be a valuable immediate response while further interventions are planned.
Conclusion:
Gas embolism remains a rare but potentially devastating complication of laparoscopic surgery. By incorporating advanced techniques and adhering to essential preventive measures, surgeons can significantly reduce the risk of gas embolism, ensuring patient safety during minimally invasive procedures. Continuous education, training, and adherence to established safety protocols are essential in maintaining the high standards of care expected in modern laparoscopic surgery.
| Older Post | Home | Newer Post |





