Cardiovascular Complications in Laparoscopic Surgery: A Revie
Introduction:
Laparoscopic surgery, also known as minimally invasive surgery, has revolutionized the field of surgery, offering numerous advantages over traditional open surgery. These advantages include smaller incisions, reduced pain and scarring, shorter hospital stays, and faster recovery times. However, despite its benefits, laparoscopic surgery can have unique cardiovascular implications and complications that are essential for surgeons, especially in regions with rapidly advancing medical fields like Gurugram, to understand and manage.
Pathophysiology:
The cardiovascular complications in laparoscopic surgery primarily arise from the insufflation of carbon dioxide (CO2) into the abdominal cavity to create a working space, known as pneumoperitoneum. The increased intra-abdominal pressure and the systemic absorption of CO2 can lead to significant physiological changes. These changes include increased systemic vascular resistance, altered venous return, and direct cardiac compression, all of which can impact cardiac output and blood pressure. Additionally, patient positioning during surgery, such as the Trendelenburg or reverse Trendelenburg positions, can further affect cardiovascular dynamics.
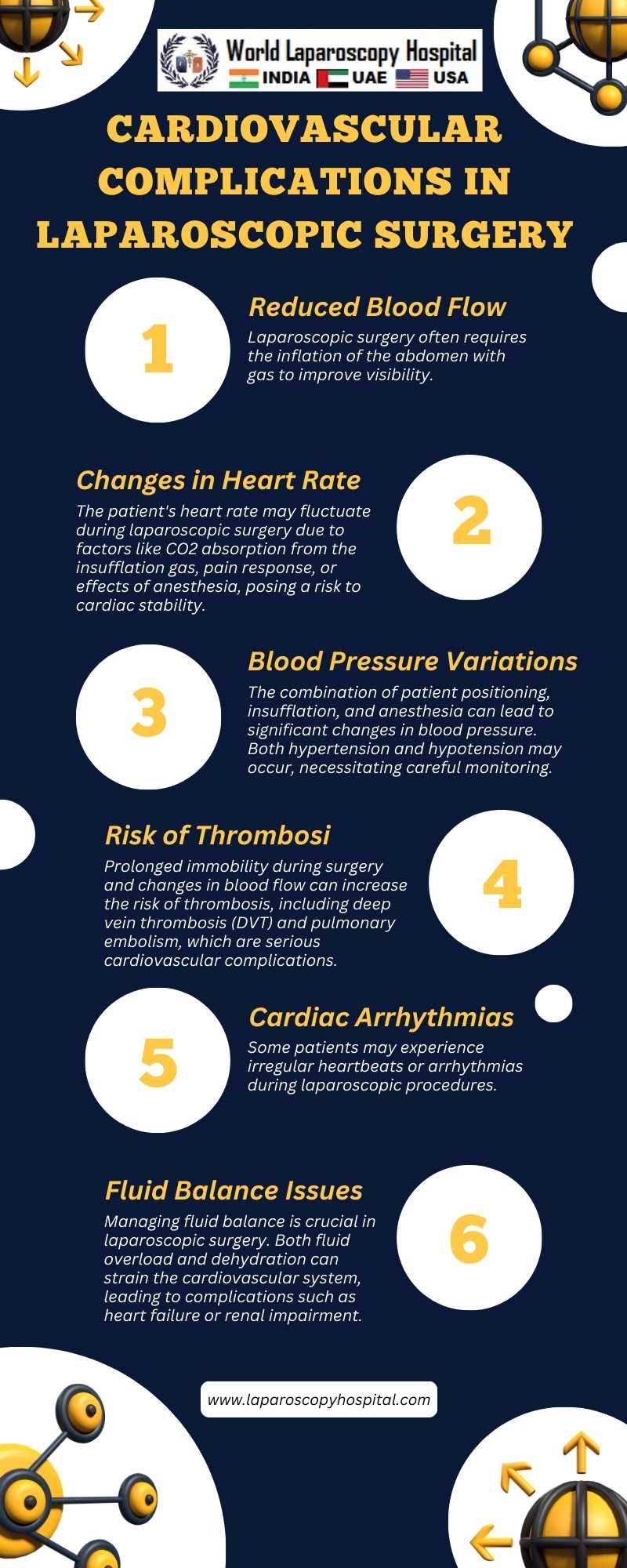
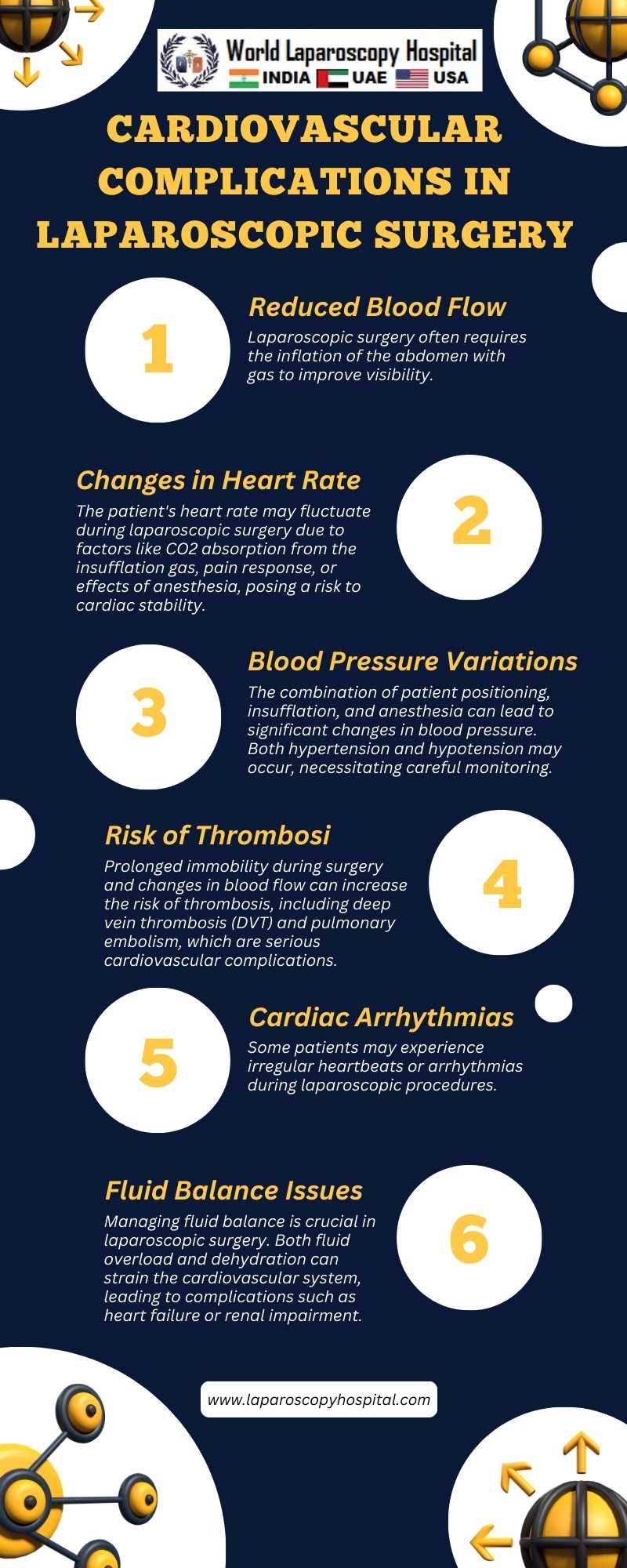
Complications:
1. Hemodynamic Changes: The establishment of pneumoperitoneum can lead to increased blood pressure and decreased cardiac output. These changes are generally well-tolerated in healthy individuals but can be detrimental in patients with pre-existing cardiac conditions.
2. Arrhythmias: The absorption of CO2 can lead to hypercarbia, which may trigger arrhythmic events, particularly in susceptible individuals.
3. Myocardial Ischemia: Patients with coronary artery disease are at an increased risk of myocardial ischemia during laparoscopic surgery due to hemodynamic stress and potential hypercarbia.
4. Venous Thromboembolism (VTE): The reduced venous return and immobilization during surgery can increase the risk of deep vein thrombosis, which can lead to pulmonary embolism, a potentially fatal complication.
Prevention and Management:
1. Preoperative Assessment: Thorough cardiovascular evaluation and optimization of pre-existing cardiac conditions are crucial before considering a patient for laparoscopic surgery.
2. Intraoperative Monitoring: Continuous monitoring of vital signs, including end-tidal CO2, can help in early detection and management of cardiovascular complications.
3. Limiting Pneumoperitoneum Pressure: Maintaining the lowest effective intra-abdominal pressure can minimize hemodynamic changes.
4. Patient Positioning: Careful positioning to avoid prolonged periods in positions that can adversely affect cardiac output is important.
5. Pharmacological Management: The use of drugs to manage arrhythmias or myocardial ischemia should be considered if necessary.
6. Early Mobilization: Encouraging early postoperative mobilization can reduce the risk of VTE.
Conclusion:
While laparoscopic surgery offers many benefits, it is not devoid of risks, particularly concerning cardiovascular health. Understanding these risks and implementing strategies for prevention and management are essential for optimizing patient outcomes. Continuous advancements in surgical techniques and patient monitoring are also crucial in mitigating these risks, particularly in dynamic medical environments like Gurugram. As the field of minimally invasive surgery evolves, so must our approaches to managing its complications, ensuring that the benefits of these procedures are not overshadowed by preventable adverse events.
Laparoscopic surgery, also known as minimally invasive surgery, has revolutionized the field of surgery, offering numerous advantages over traditional open surgery. These advantages include smaller incisions, reduced pain and scarring, shorter hospital stays, and faster recovery times. However, despite its benefits, laparoscopic surgery can have unique cardiovascular implications and complications that are essential for surgeons, especially in regions with rapidly advancing medical fields like Gurugram, to understand and manage.
Pathophysiology:
The cardiovascular complications in laparoscopic surgery primarily arise from the insufflation of carbon dioxide (CO2) into the abdominal cavity to create a working space, known as pneumoperitoneum. The increased intra-abdominal pressure and the systemic absorption of CO2 can lead to significant physiological changes. These changes include increased systemic vascular resistance, altered venous return, and direct cardiac compression, all of which can impact cardiac output and blood pressure. Additionally, patient positioning during surgery, such as the Trendelenburg or reverse Trendelenburg positions, can further affect cardiovascular dynamics.
Complications:
1. Hemodynamic Changes: The establishment of pneumoperitoneum can lead to increased blood pressure and decreased cardiac output. These changes are generally well-tolerated in healthy individuals but can be detrimental in patients with pre-existing cardiac conditions.
2. Arrhythmias: The absorption of CO2 can lead to hypercarbia, which may trigger arrhythmic events, particularly in susceptible individuals.
3. Myocardial Ischemia: Patients with coronary artery disease are at an increased risk of myocardial ischemia during laparoscopic surgery due to hemodynamic stress and potential hypercarbia.
4. Venous Thromboembolism (VTE): The reduced venous return and immobilization during surgery can increase the risk of deep vein thrombosis, which can lead to pulmonary embolism, a potentially fatal complication.
Prevention and Management:
1. Preoperative Assessment: Thorough cardiovascular evaluation and optimization of pre-existing cardiac conditions are crucial before considering a patient for laparoscopic surgery.
2. Intraoperative Monitoring: Continuous monitoring of vital signs, including end-tidal CO2, can help in early detection and management of cardiovascular complications.
3. Limiting Pneumoperitoneum Pressure: Maintaining the lowest effective intra-abdominal pressure can minimize hemodynamic changes.
4. Patient Positioning: Careful positioning to avoid prolonged periods in positions that can adversely affect cardiac output is important.
5. Pharmacological Management: The use of drugs to manage arrhythmias or myocardial ischemia should be considered if necessary.
6. Early Mobilization: Encouraging early postoperative mobilization can reduce the risk of VTE.
Conclusion:
While laparoscopic surgery offers many benefits, it is not devoid of risks, particularly concerning cardiovascular health. Understanding these risks and implementing strategies for prevention and management are essential for optimizing patient outcomes. Continuous advancements in surgical techniques and patient monitoring are also crucial in mitigating these risks, particularly in dynamic medical environments like Gurugram. As the field of minimally invasive surgery evolves, so must our approaches to managing its complications, ensuring that the benefits of these procedures are not overshadowed by preventable adverse events.
2 COMMENTS
Dr. K K Dwivedi
#1
Jan 27th, 2024 9:04 am
Laparoscopic surgery's revolutionary impact is evident in smaller incisions, reduced pain, and faster recovery. Yet, cardiovascular implications pose unique challenges. Surgeons, especially in rapidly advancing medical regions like Gurugram, must comprehend and manage these complexities.
Dr. Anurag Jaiswal
#2
Feb 27th, 2024 5:13 pm
Laparoscopic surgery, though beneficial, carries cardiovascular risks. Awareness and preventive strategies are vital for patient well-being. Ongoing advances in techniques and monitoring, especially in dynamic settings like Gurugram, mitigate risks. Evolving management approaches ensure the benefits outweigh potential adverse events.
| Older Post | Home | Newer Post |





