Innovative Approaches in Laparoscopic Tracheoesophageal Fistula Repair
Innovative Approaches in Laparoscopic Tracheoesophageal Fistula Repair
Tracheoesophageal fistulas (TEFs) are complex congenital or acquired anomalies that demand meticulous surgical intervention. Historically, open surgical techniques have been the go-to approach for addressing these challenging conditions. However, in recent years, the landscape of TEF repair has seen a remarkable transformation with the advent of innovative laparoscopic approaches. These minimally invasive techniques have not only revolutionized patient care but have also presented surgeons with new tools and strategies to tackle TEFs more effectively.
This article delves into the world of innovative approaches in laparoscopic tracheoesophageal fistula repair, shedding light on the benefits, challenges, and promising outcomes associated with these groundbreaking methods.
The Evolution of TEF Repair: From Open to Laparoscopic
Traditionally, TEF repair involved extensive open surgical procedures, which often required large incisions, prolonged hospital stays, and lengthy recovery periods. These techniques, while effective, were associated with higher rates of morbidity and complications. Laparoscopic TEF repair emerged as a paradigm shift in this field, offering several advantages over its open counterpart.
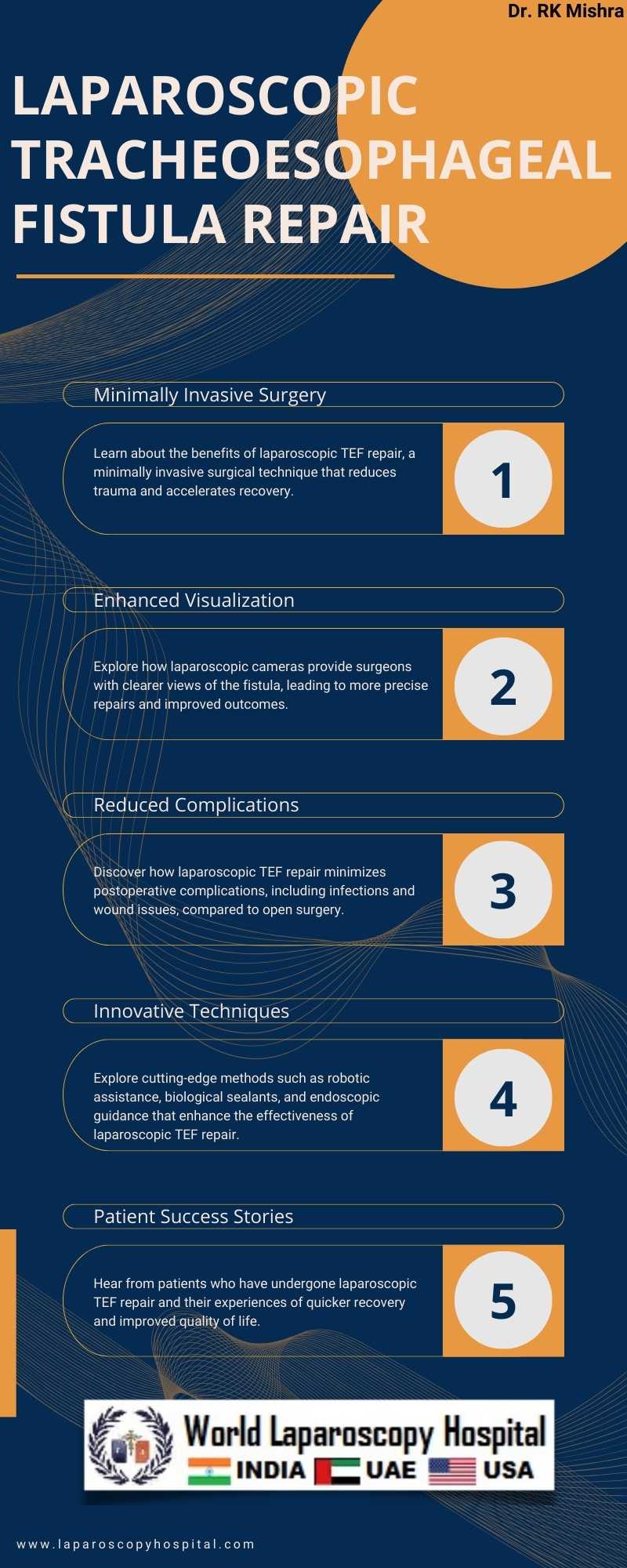
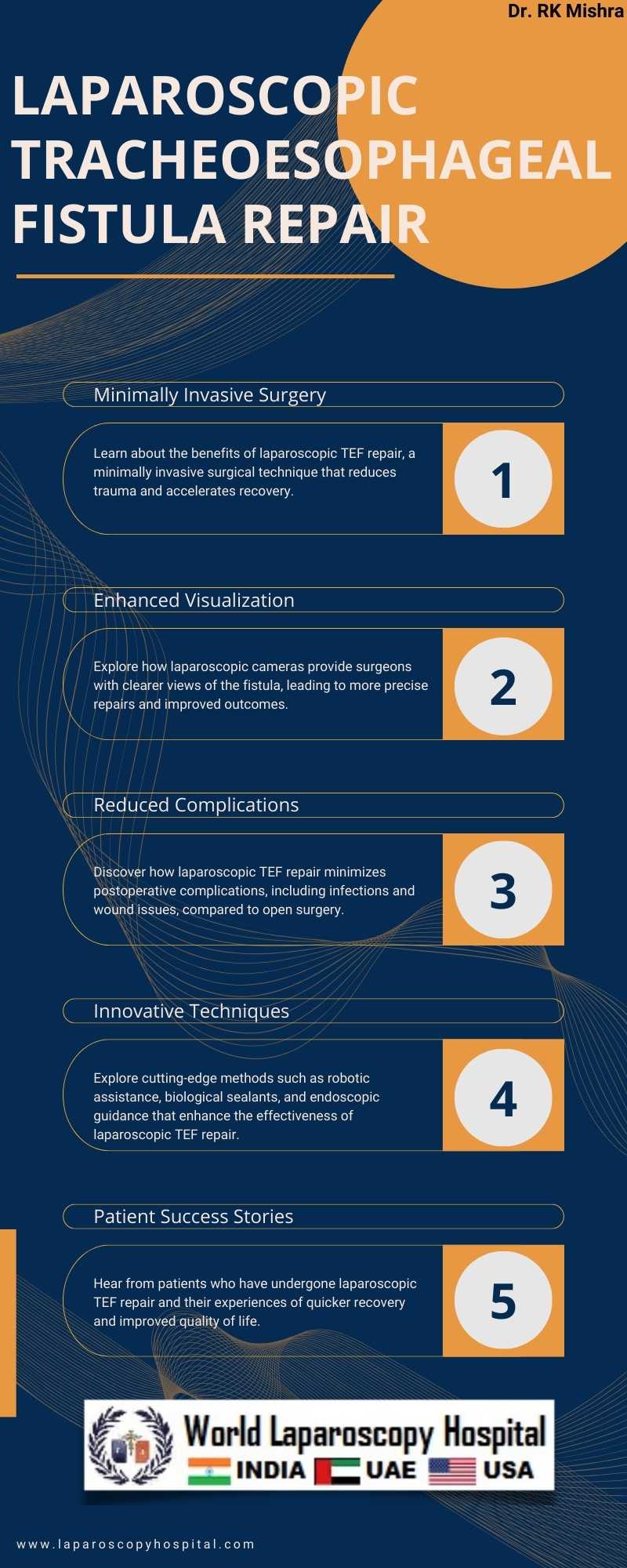
Minimally Invasive Precision
Laparoscopic TEF repair is characterized by its minimally invasive nature. Surgeons make small incisions and employ specialized instruments and a camera (laparoscope) to access and repair the fistula. This approach significantly reduces surgical trauma, postoperative pain, and recovery time. Patients can often return to their normal activities more swiftly, contributing to an improved overall quality of life.
Enhanced Visualization
One of the key elements in laparoscopic TEF repair is the enhanced visualization provided by the laparoscope. Surgeons can magnify the surgical field, allowing for precise identification and closure of the fistula. This heightened clarity aids in avoiding injury to nearby structures and ensuring a more successful repair.
Reduced Postoperative Complications
Compared to open surgery, laparoscopic TEF repair has shown a decrease in postoperative complications such as wound infections and hernias. The smaller incisions are less prone to infection, and patients are at a lower risk of developing complications related to long incisions, such as wound dehiscence.
Innovative Techniques in Laparoscopic TEF Repair
1. Fundoplication Adjunct: Laparoscopic fundoplication, a procedure to treat gastroesophageal reflux disease (GERD), has been integrated into TEF repair. This innovative approach not only addresses the TEF but also manages associated conditions like GERD simultaneously.
2. Biological Sealants: The use of biological sealants during laparoscopic TEF repair has gained traction. These sealants aid in reinforcing the closure of the fistula and reducing the risk of postoperative leakage.
3. Robotic Assistance: Some surgeons have begun to explore the use of robotic-assisted laparoscopic techniques for TEF repair. The robotic system offers enhanced dexterity and precision, making it particularly valuable in challenging cases.
4. Endoscopic Guidance: Combining endoscopic and laparoscopic techniques allows for better assessment of the entire esophagus, enabling surgeons to identify and treat additional issues beyond the TEF.
Challenges and Considerations
While laparoscopic TEF repair holds great promise, it is not without challenges. Patient selection is crucial, and not all TEFs are suitable for laparoscopic repair. Some complex cases may still require open surgery. Additionally, there is a learning curve associated with laparoscopic techniques, necessitating specialized training for surgeons.
Conclusion
Innovative approaches in laparoscopic tracheoesophageal fistula repair have ushered in a new era of patient care and surgical precision. These techniques offer numerous benefits, including reduced trauma, improved visualization, and fewer postoperative complications. As technology and surgical expertise continue to advance, it is likely that laparoscopic TEF repair will become the preferred method for an even wider range of cases. With ongoing research and innovation, the future of TEF repair is indeed promising, offering hope and improved outcomes for patients facing this challenging condition. Surgeons in Gurugram and around the world are at the forefront of this transformative journey, working tirelessly to refine and expand the boundaries of laparoscopic TEF repair.
Tracheoesophageal fistulas (TEFs) are complex congenital or acquired anomalies that demand meticulous surgical intervention. Historically, open surgical techniques have been the go-to approach for addressing these challenging conditions. However, in recent years, the landscape of TEF repair has seen a remarkable transformation with the advent of innovative laparoscopic approaches. These minimally invasive techniques have not only revolutionized patient care but have also presented surgeons with new tools and strategies to tackle TEFs more effectively.
This article delves into the world of innovative approaches in laparoscopic tracheoesophageal fistula repair, shedding light on the benefits, challenges, and promising outcomes associated with these groundbreaking methods.
The Evolution of TEF Repair: From Open to Laparoscopic
Traditionally, TEF repair involved extensive open surgical procedures, which often required large incisions, prolonged hospital stays, and lengthy recovery periods. These techniques, while effective, were associated with higher rates of morbidity and complications. Laparoscopic TEF repair emerged as a paradigm shift in this field, offering several advantages over its open counterpart.
Minimally Invasive Precision
Laparoscopic TEF repair is characterized by its minimally invasive nature. Surgeons make small incisions and employ specialized instruments and a camera (laparoscope) to access and repair the fistula. This approach significantly reduces surgical trauma, postoperative pain, and recovery time. Patients can often return to their normal activities more swiftly, contributing to an improved overall quality of life.
Enhanced Visualization
One of the key elements in laparoscopic TEF repair is the enhanced visualization provided by the laparoscope. Surgeons can magnify the surgical field, allowing for precise identification and closure of the fistula. This heightened clarity aids in avoiding injury to nearby structures and ensuring a more successful repair.
Reduced Postoperative Complications
Compared to open surgery, laparoscopic TEF repair has shown a decrease in postoperative complications such as wound infections and hernias. The smaller incisions are less prone to infection, and patients are at a lower risk of developing complications related to long incisions, such as wound dehiscence.
Innovative Techniques in Laparoscopic TEF Repair
1. Fundoplication Adjunct: Laparoscopic fundoplication, a procedure to treat gastroesophageal reflux disease (GERD), has been integrated into TEF repair. This innovative approach not only addresses the TEF but also manages associated conditions like GERD simultaneously.
2. Biological Sealants: The use of biological sealants during laparoscopic TEF repair has gained traction. These sealants aid in reinforcing the closure of the fistula and reducing the risk of postoperative leakage.
3. Robotic Assistance: Some surgeons have begun to explore the use of robotic-assisted laparoscopic techniques for TEF repair. The robotic system offers enhanced dexterity and precision, making it particularly valuable in challenging cases.
4. Endoscopic Guidance: Combining endoscopic and laparoscopic techniques allows for better assessment of the entire esophagus, enabling surgeons to identify and treat additional issues beyond the TEF.
Challenges and Considerations
While laparoscopic TEF repair holds great promise, it is not without challenges. Patient selection is crucial, and not all TEFs are suitable for laparoscopic repair. Some complex cases may still require open surgery. Additionally, there is a learning curve associated with laparoscopic techniques, necessitating specialized training for surgeons.
Conclusion
Innovative approaches in laparoscopic tracheoesophageal fistula repair have ushered in a new era of patient care and surgical precision. These techniques offer numerous benefits, including reduced trauma, improved visualization, and fewer postoperative complications. As technology and surgical expertise continue to advance, it is likely that laparoscopic TEF repair will become the preferred method for an even wider range of cases. With ongoing research and innovation, the future of TEF repair is indeed promising, offering hope and improved outcomes for patients facing this challenging condition. Surgeons in Gurugram and around the world are at the forefront of this transformative journey, working tirelessly to refine and expand the boundaries of laparoscopic TEF repair.
2 COMMENTS
Dr. Abhinav Gupta
#1
Dec 3rd, 2023 8:48 am
Tracheoesophageal fistulas (TEFs) present complex challenges, traditionally addressed by open surgery. However, recent years have witnessed a transformative shift with innovative laparoscopic approaches, revolutionizing patient care and providing surgeons effective tools. This article explores the benefits, challenges, and promising outcomes of these groundbreaking methods.
Dr. Abhay Pratap
#2
Dec 7th, 2023 3:44 pm
Tracheoesophageal fistulas (TEFs), intricate anomalies, historically addressed with open surgery, undergo a transformative shift with innovative laparoscopic approaches. This article explores the world of laparoscopic TEF repair, highlighting benefits, challenges, and promising outcomes.
| Older Post | Home | Newer Post |

