Hyperglycemic hyperosmolar state: A serious complication of diabetes that can be precipitated by surgery.
Hyperglycemic hyperosmolar state: A serious complication of diabetes that can be precipitated by surgery.
Introduction
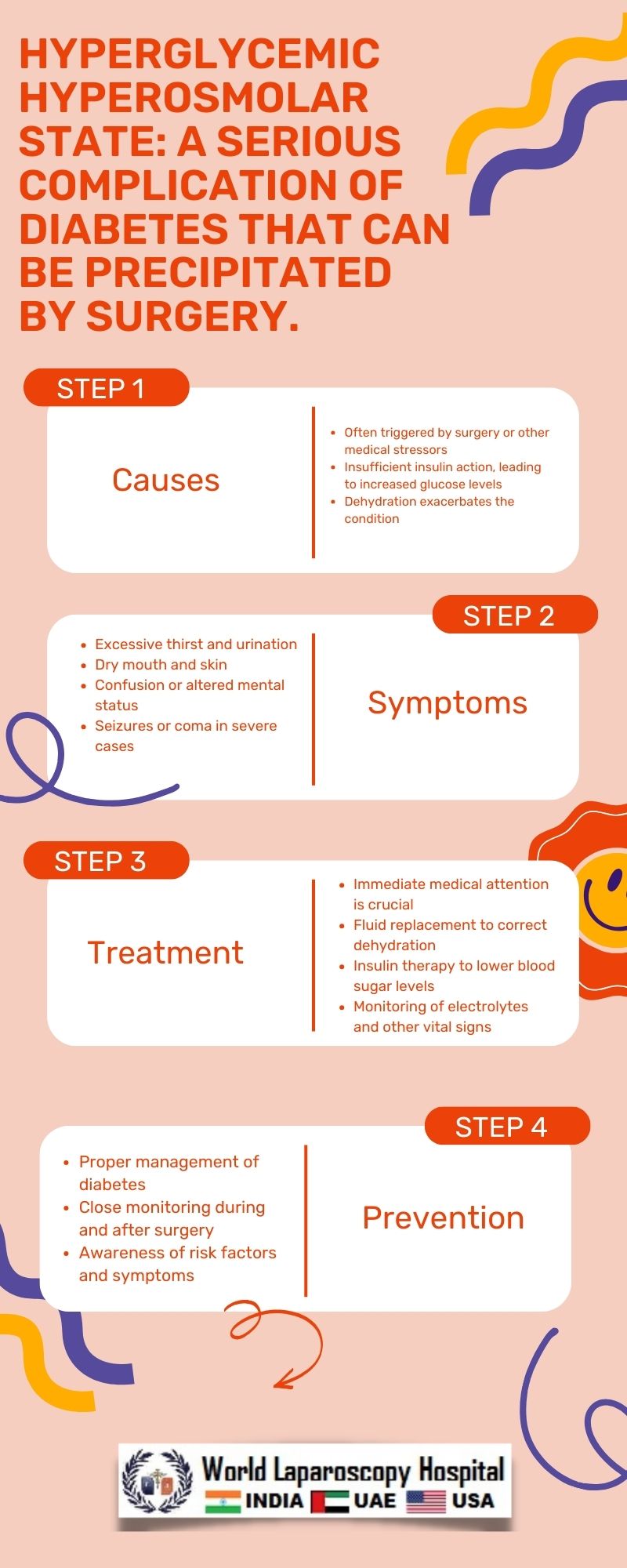
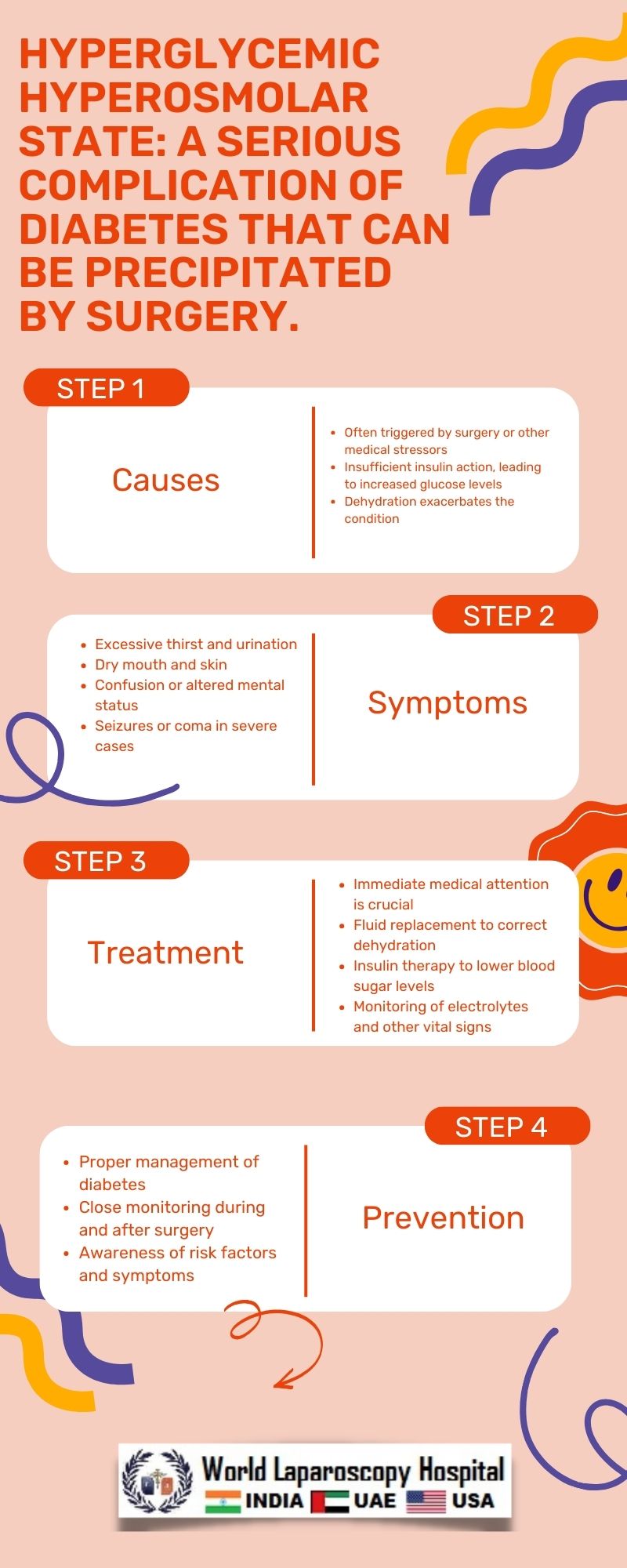
Diabetes mellitus is a chronic metabolic disorder characterized by high blood glucose levels, either due to inadequate insulin production or the body's inability to use insulin effectively. It affects millions of people worldwide and can lead to various complications if not properly managed. One such complication is the hyperglycemic hyperosmolar state (HHS), a life-threatening condition that can be precipitated by surgery.
Understanding Diabetes Mellitus
Diabetes mellitus is classified into several types, with the most common being type 1 and type 2 diabetes. In type 1 diabetes, the body's immune system attacks and destroys the insulin-producing beta cells in the pancreas, leading to a lack of insulin production. Type 2 diabetes, on the other hand, is characterized by insulin resistance, where the body's cells do not respond effectively to insulin, leading to elevated blood glucose levels.
Hyperglycemic Hyperosmolar State (HHS)
HHS, also known as hyperosmolar hyperglycemic nonketotic syndrome (HHNS), is a severe complication of diabetes mellitus characterized by extremely high blood glucose levels, dehydration, and altered mental status. Unlike diabetic ketoacidosis (DKA), another complication of diabetes characterized by ketosis and acidosis, HHS is characterized by the absence of significant ketosis and acidosis.
Precipitating Factors of HHS
Several factors can precipitate or trigger HHS in individuals with diabetes, with surgery being one of the major triggers. During surgery, the body undergoes significant stress, leading to the release of stress hormones such as cortisol and catecholamines. These hormones can increase blood glucose levels by stimulating the liver to release glucose and reducing the body's sensitivity to insulin.
Mechanism of HHS Development
The development of HHS during surgery involves a complex interplay of various factors. The stress response to surgery leads to increased production of glucose by the liver and decreased utilization of glucose by peripheral tissues. This, combined with the insulin resistance commonly seen in individuals with diabetes, results in a rapid rise in blood glucose levels.
Clinical Presentation of HHS
The clinical presentation of HHS is characterized by severe hyperglycemia (blood glucose levels typically exceeding 600 mg/dL), dehydration, and altered mental status. Patients may present with symptoms such as excessive thirst, dry mouth, weakness, confusion, and in severe cases, coma. Laboratory findings typically include hyperglycemia, hyperosmolality, and dehydration.
Diagnosis of HHS
Diagnosis of HHS is based on clinical and laboratory findings. Blood tests revealing severe hyperglycemia (blood glucose >600 mg/dL), elevated serum osmolality (>320 mOsm/kg), and absence of significant ketosis are indicative of HHS. Other laboratory findings may include elevated serum sodium levels, increased blood urea nitrogen (BUN), and creatinine levels.
Management of HHS
The management of HHS involves several key components, including fluid resuscitation, correction of electrolyte imbalances, insulin therapy, and identification and treatment of underlying precipitating factors. Fluid resuscitation is crucial to correct dehydration and restore intravascular volume, typically with isotonic saline. Insulin therapy is essential to lower blood glucose levels and reverse the hyperosmolar state.
Prevention of HHS in Surgical Patients with Diabetes
Prevention of HHS in surgical patients with diabetes involves careful preoperative evaluation and optimization of glycemic control. Patients with diabetes undergoing surgery should have their blood glucose levels closely monitored before, during, and after surgery. In addition, measures should be taken to minimize stress responses to surgery, such as adequate pain control and perioperative glucose management.
Conclusion
Hyperglycemic hyperosmolar state is a serious complication of diabetes that can be precipitated by surgery. It is characterized by severe hyperglycemia, dehydration, and altered mental status. Early recognition and prompt management are essential to prevent complications and improve outcomes in affected patients. Healthcare providers should be vigilant in identifying patients at risk for HHS and implementing appropriate preventive measures in the perioperative period.
Introduction
Diabetes mellitus is a chronic metabolic disorder characterized by high blood glucose levels, either due to inadequate insulin production or the body's inability to use insulin effectively. It affects millions of people worldwide and can lead to various complications if not properly managed. One such complication is the hyperglycemic hyperosmolar state (HHS), a life-threatening condition that can be precipitated by surgery.
Understanding Diabetes Mellitus
Diabetes mellitus is classified into several types, with the most common being type 1 and type 2 diabetes. In type 1 diabetes, the body's immune system attacks and destroys the insulin-producing beta cells in the pancreas, leading to a lack of insulin production. Type 2 diabetes, on the other hand, is characterized by insulin resistance, where the body's cells do not respond effectively to insulin, leading to elevated blood glucose levels.
Hyperglycemic Hyperosmolar State (HHS)
HHS, also known as hyperosmolar hyperglycemic nonketotic syndrome (HHNS), is a severe complication of diabetes mellitus characterized by extremely high blood glucose levels, dehydration, and altered mental status. Unlike diabetic ketoacidosis (DKA), another complication of diabetes characterized by ketosis and acidosis, HHS is characterized by the absence of significant ketosis and acidosis.
Precipitating Factors of HHS
Several factors can precipitate or trigger HHS in individuals with diabetes, with surgery being one of the major triggers. During surgery, the body undergoes significant stress, leading to the release of stress hormones such as cortisol and catecholamines. These hormones can increase blood glucose levels by stimulating the liver to release glucose and reducing the body's sensitivity to insulin.
Mechanism of HHS Development
The development of HHS during surgery involves a complex interplay of various factors. The stress response to surgery leads to increased production of glucose by the liver and decreased utilization of glucose by peripheral tissues. This, combined with the insulin resistance commonly seen in individuals with diabetes, results in a rapid rise in blood glucose levels.
Clinical Presentation of HHS
The clinical presentation of HHS is characterized by severe hyperglycemia (blood glucose levels typically exceeding 600 mg/dL), dehydration, and altered mental status. Patients may present with symptoms such as excessive thirst, dry mouth, weakness, confusion, and in severe cases, coma. Laboratory findings typically include hyperglycemia, hyperosmolality, and dehydration.
Diagnosis of HHS
Diagnosis of HHS is based on clinical and laboratory findings. Blood tests revealing severe hyperglycemia (blood glucose >600 mg/dL), elevated serum osmolality (>320 mOsm/kg), and absence of significant ketosis are indicative of HHS. Other laboratory findings may include elevated serum sodium levels, increased blood urea nitrogen (BUN), and creatinine levels.
Management of HHS
The management of HHS involves several key components, including fluid resuscitation, correction of electrolyte imbalances, insulin therapy, and identification and treatment of underlying precipitating factors. Fluid resuscitation is crucial to correct dehydration and restore intravascular volume, typically with isotonic saline. Insulin therapy is essential to lower blood glucose levels and reverse the hyperosmolar state.
Prevention of HHS in Surgical Patients with Diabetes
Prevention of HHS in surgical patients with diabetes involves careful preoperative evaluation and optimization of glycemic control. Patients with diabetes undergoing surgery should have their blood glucose levels closely monitored before, during, and after surgery. In addition, measures should be taken to minimize stress responses to surgery, such as adequate pain control and perioperative glucose management.
Conclusion
Hyperglycemic hyperosmolar state is a serious complication of diabetes that can be precipitated by surgery. It is characterized by severe hyperglycemia, dehydration, and altered mental status. Early recognition and prompt management are essential to prevent complications and improve outcomes in affected patients. Healthcare providers should be vigilant in identifying patients at risk for HHS and implementing appropriate preventive measures in the perioperative period.
1 COMMENTS
Dr. Gagandeep Thukral
#1
Feb 26th, 2024 5:53 am
Hyperglycemic hyperosmolar state, a perilous diabetes complication, may arise post-surgery with severe hyperglycemia and dehydration. Timely recognition and management are critical to avert complications and enhance outcomes. Healthcare providers must vigilantly identify at-risk patients and employ preventive measures perioperatively.
| Older Post | Home | Newer Post |


