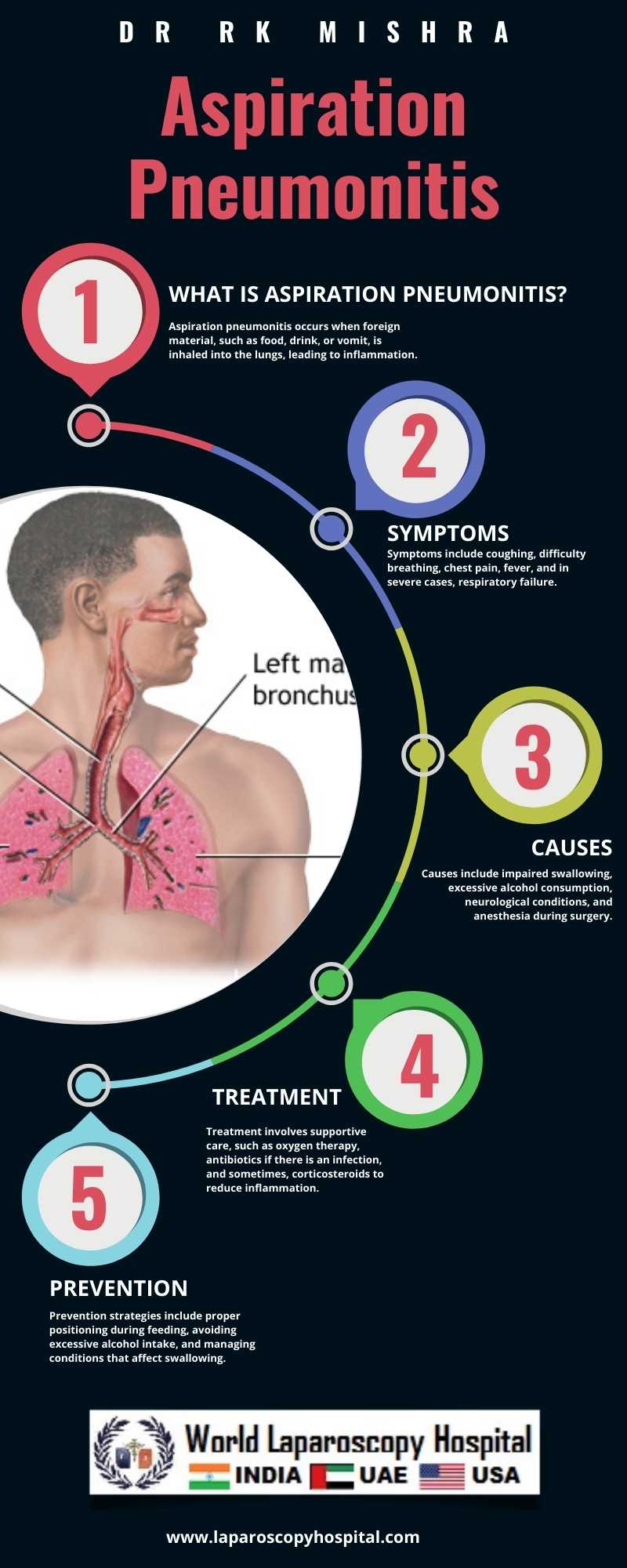
Aspiration pneumonitis: Lung inflammation due to inhaling foreign material, a risk during or after surgery
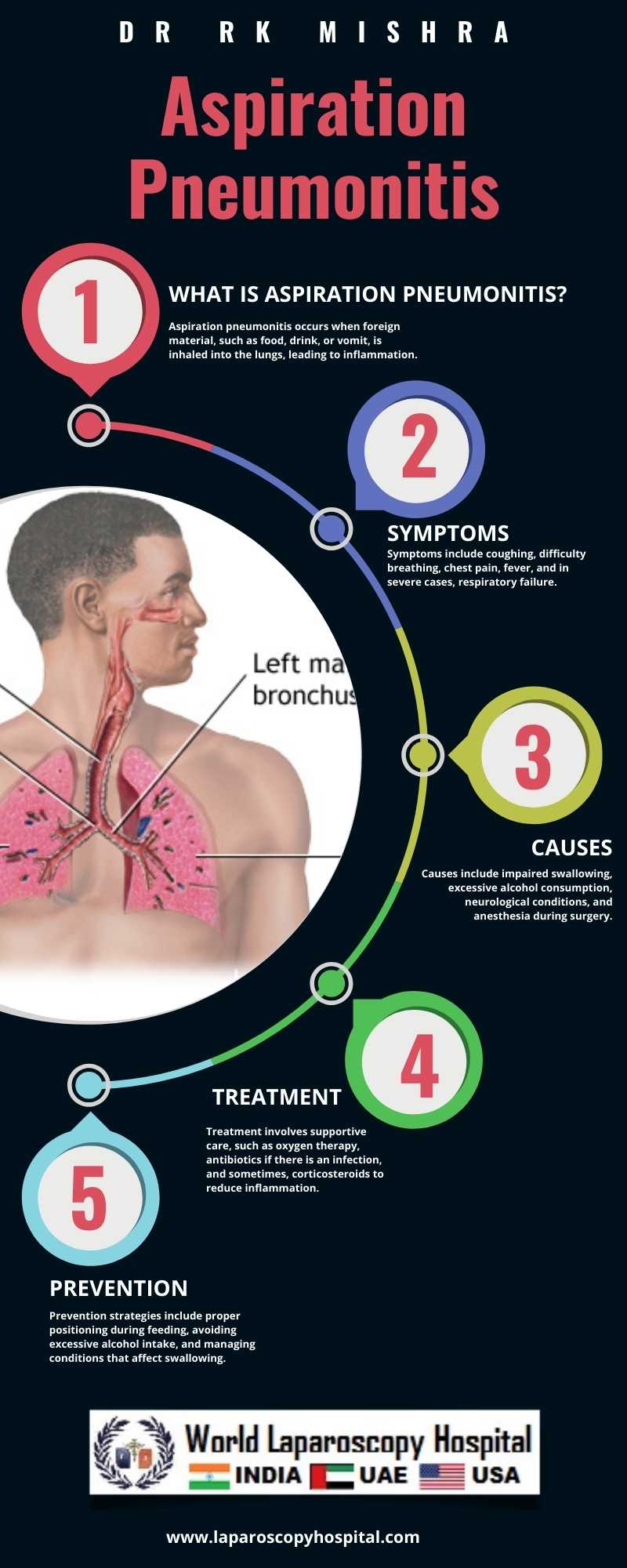
Aspiration pneumonitis, also known as chemical pneumonitis, is a condition characterized by inflammation of the lungs caused by inhaling foreign material, such as gastric contents or food particles, into the respiratory tract. This condition poses a significant risk during or after surgery, especially in patients under anesthesia or those with altered consciousness.
During surgical procedures, patients are often placed under general anesthesia, which causes a temporary loss of protective airway reflexes. This increases the risk of aspiration, as the normal cough and gag reflexes that prevent foreign material from entering the lungs are suppressed. Additionally, patients undergoing surgery may have reduced mobility or be in a position that facilitates the entry of gastric contents into the lungs, further increasing the risk of aspiration pneumonitis.
After surgery, patients may experience nausea, vomiting, or impaired swallowing, which can also increase the risk of aspiration. Other factors that contribute to the development of aspiration pneumonitis include advanced age, obesity, gastroesophageal reflux disease (GERD), and conditions that affect the esophagus or stomach.
The clinical presentation of aspiration pneumonitis can vary widely, ranging from mild respiratory symptoms to severe acute respiratory distress syndrome (ARDS). Common symptoms include cough, shortness of breath, chest pain, and fever. In severe cases, patients may develop hypoxemia, respiratory failure, and septic shock, which can be life-threatening.
Diagnosis of aspiration pneumonitis is based on a combination of clinical findings, imaging studies (such as chest X-ray or CT scan), and laboratory tests. Treatment depends on the severity of the condition but often includes supportive care, such as supplemental oxygen, mechanical ventilation, and antibiotics to treat secondary infections. In some cases, bronchoscopy may be performed to remove aspirated material from the airways.
Prevention of aspiration pneumonitis is key, especially in high-risk patients. This includes proper patient positioning during surgery, maintaining a clear airway, and minimizing the risk of regurgitation or vomiting. Patients at high risk of aspiration may also benefit from the use of medications that reduce gastric acidity or promote gastric emptying.
Conclusion:
Aspiration pneumonitis is a serious complication that can occur during or after surgery, particularly in patients with risk factors such as altered consciousness, advanced age, or GERD. Early recognition and management are essential to prevent complications and improve outcomes in affected patients.
During surgical procedures, patients are often placed under general anesthesia, which causes a temporary loss of protective airway reflexes. This increases the risk of aspiration, as the normal cough and gag reflexes that prevent foreign material from entering the lungs are suppressed. Additionally, patients undergoing surgery may have reduced mobility or be in a position that facilitates the entry of gastric contents into the lungs, further increasing the risk of aspiration pneumonitis.
After surgery, patients may experience nausea, vomiting, or impaired swallowing, which can also increase the risk of aspiration. Other factors that contribute to the development of aspiration pneumonitis include advanced age, obesity, gastroesophageal reflux disease (GERD), and conditions that affect the esophagus or stomach.
The clinical presentation of aspiration pneumonitis can vary widely, ranging from mild respiratory symptoms to severe acute respiratory distress syndrome (ARDS). Common symptoms include cough, shortness of breath, chest pain, and fever. In severe cases, patients may develop hypoxemia, respiratory failure, and septic shock, which can be life-threatening.
Diagnosis of aspiration pneumonitis is based on a combination of clinical findings, imaging studies (such as chest X-ray or CT scan), and laboratory tests. Treatment depends on the severity of the condition but often includes supportive care, such as supplemental oxygen, mechanical ventilation, and antibiotics to treat secondary infections. In some cases, bronchoscopy may be performed to remove aspirated material from the airways.
Prevention of aspiration pneumonitis is key, especially in high-risk patients. This includes proper patient positioning during surgery, maintaining a clear airway, and minimizing the risk of regurgitation or vomiting. Patients at high risk of aspiration may also benefit from the use of medications that reduce gastric acidity or promote gastric emptying.
Conclusion:
Aspiration pneumonitis is a serious complication that can occur during or after surgery, particularly in patients with risk factors such as altered consciousness, advanced age, or GERD. Early recognition and management are essential to prevent complications and improve outcomes in affected patients.
1 COMMENTS
Dr. Pratibha Mohan
#1
May 10th, 2024 8:32 pm
General anesthesia during surgery temporarily suppresses protective airway reflexes, heightening the risk of aspiration. Reduced mobility or positioning can exacerbate this risk, leading to aspiration pneumonitis. Vigilant monitoring and preventive measures are paramount in mitigating complications.
| Older Post | Home | Newer Post |


